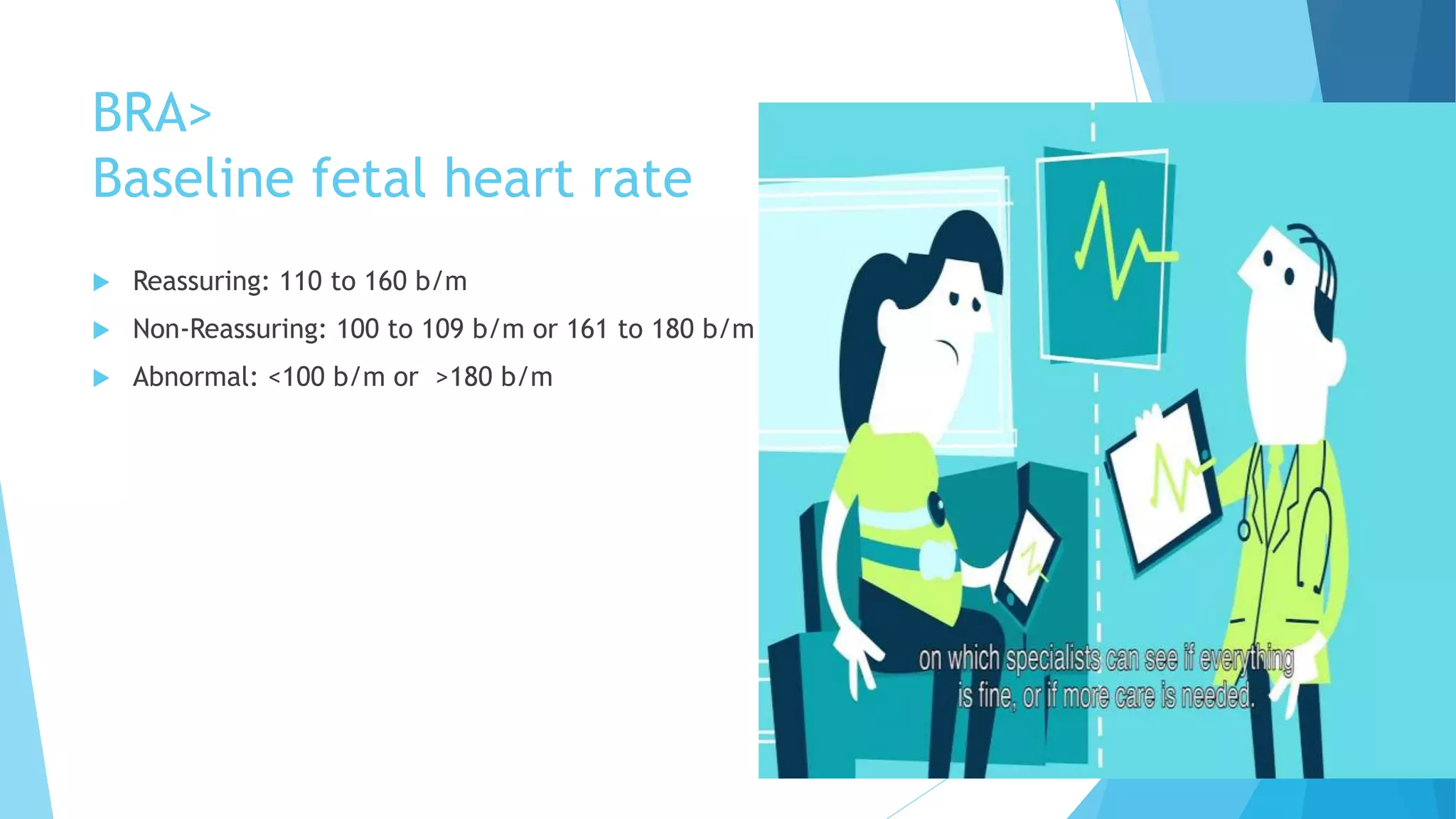
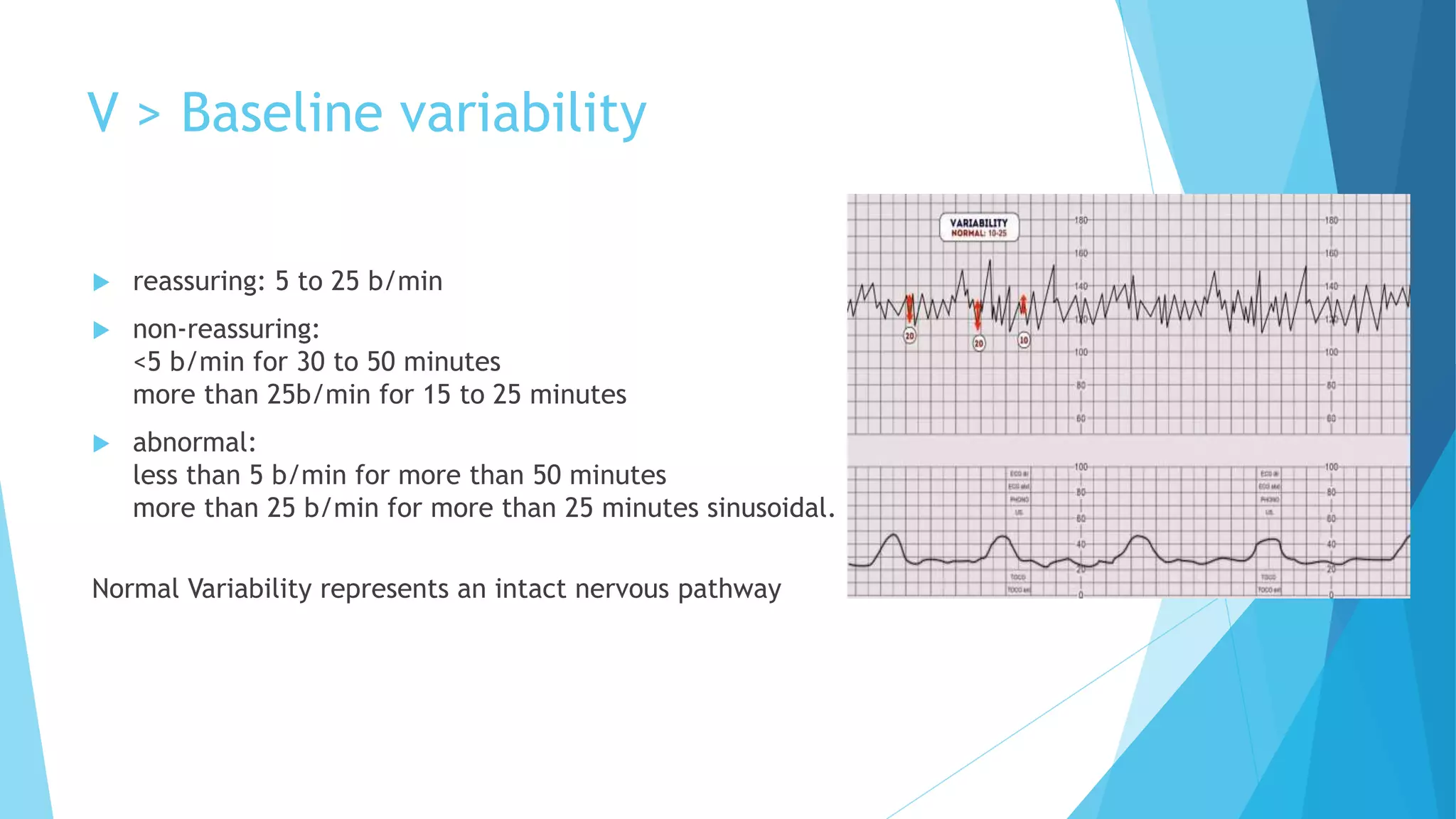
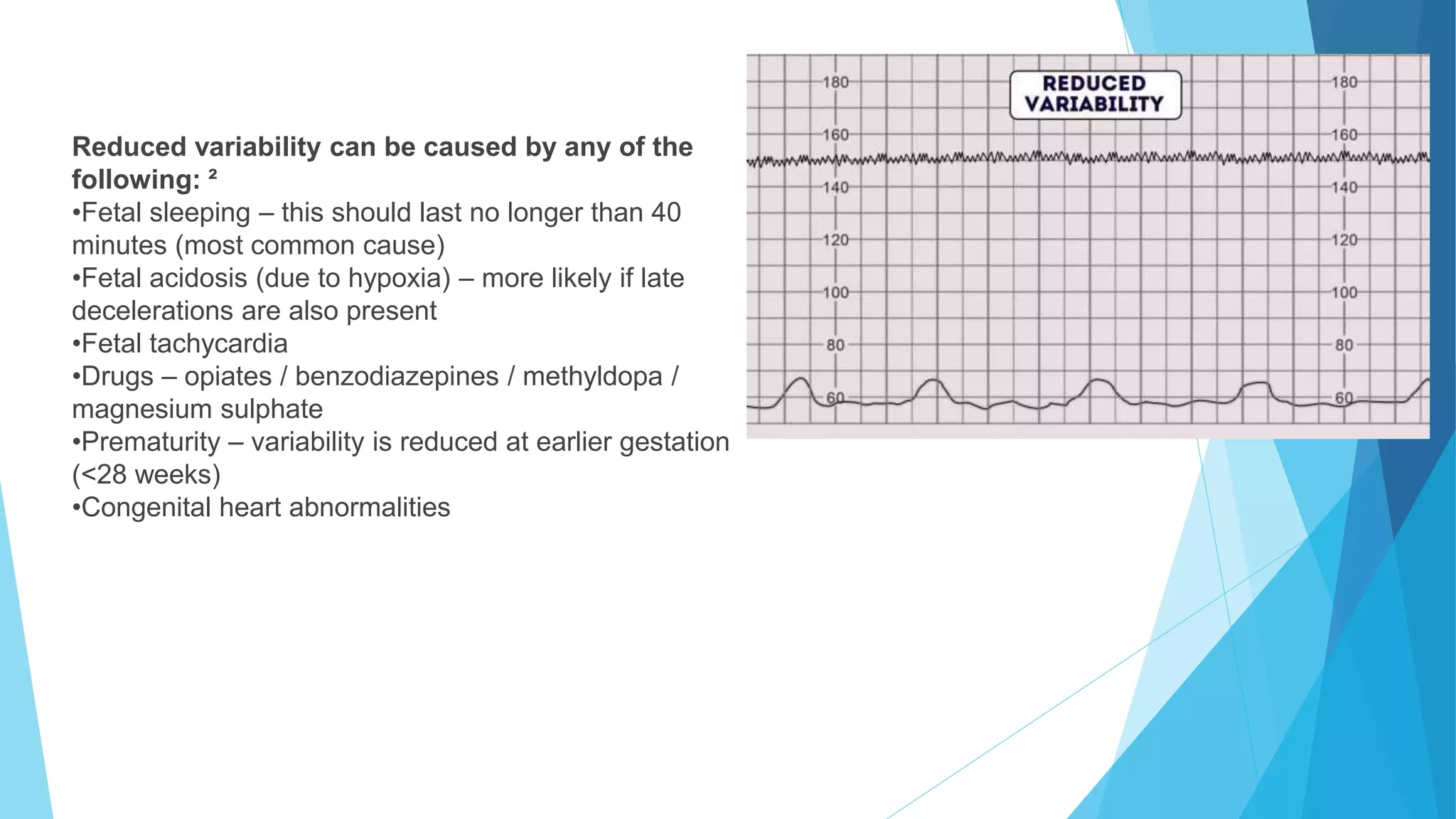
This document discusses cardiotocography (CTG), which is a method for electronic fetal monitoring. It outlines the basic patterns seen on a CTG including baseline heart rate, variability, accelerations, and decelerations. It then describes how to interpret each component of a CTG reading based on whether findings are reassuring, non-reassuring, or abnormal. Management recommendations are provided depending on the CTG category of normal, suspicious, pathological, or need for urgent intervention. Conservative measures that can be tried include changing the mother's position, giving intravenous fluids, and reducing uterine contractions.