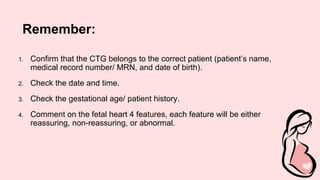
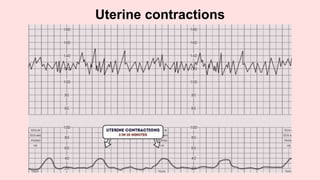
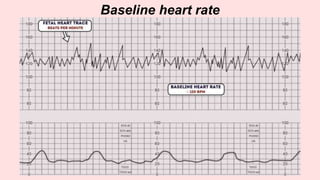
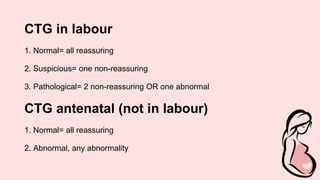
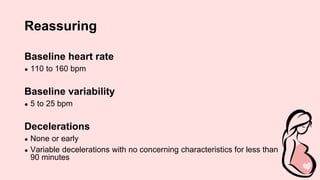
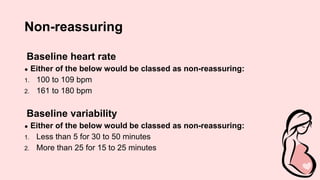
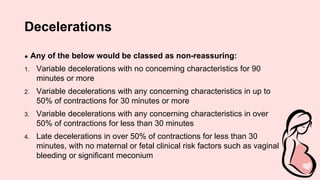
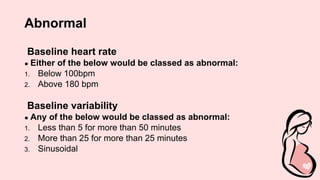
Cardiotocography (CTG) is a technique used to monitor the fetal heart rate and uterine contractions during labor. It involves placing transducers on the pregnant woman's abdomen to record this data. CTG readings are interpreted using a structured method called DR C BRAVADO, which evaluates the define risk, contractions, baseline rate, variability, accelerations, decelerations, and provides an overall impression. An abnormal CTG may indicate fetal distress and the need for further investigation or intervention during delivery.