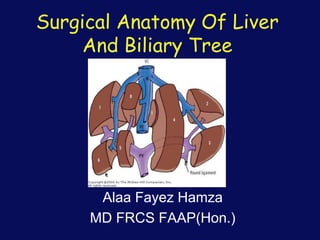
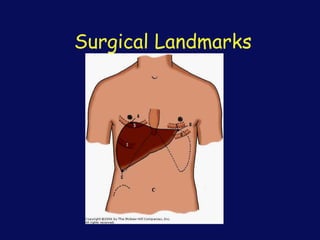
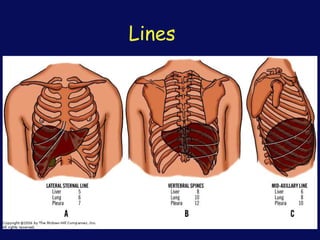
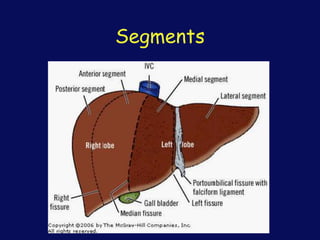
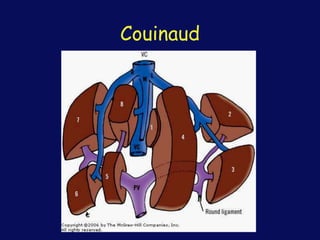
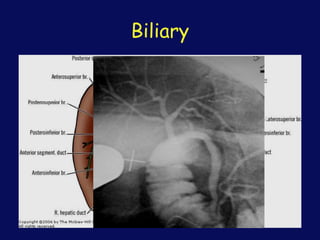
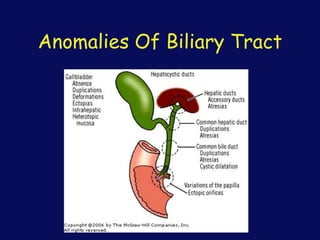
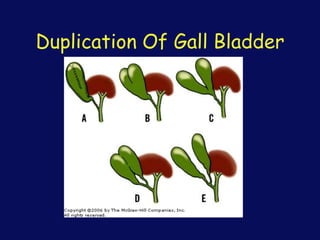
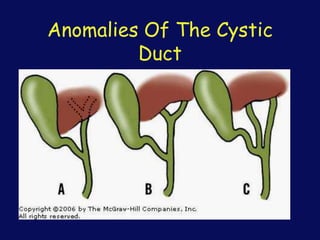
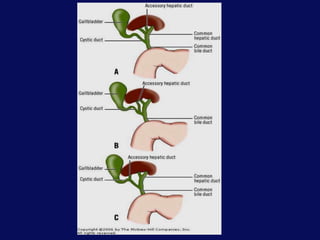
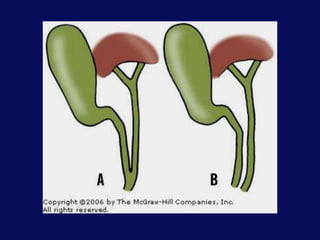
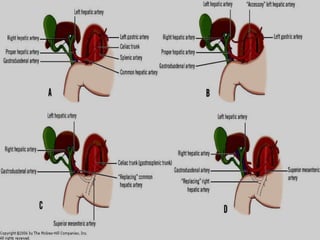
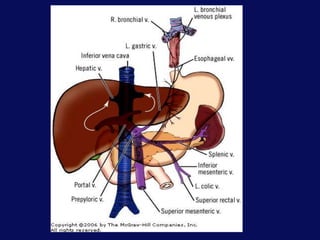
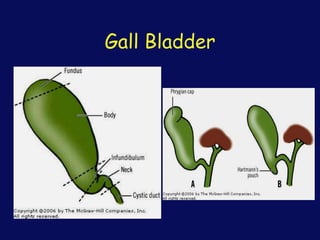
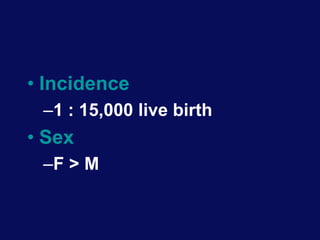
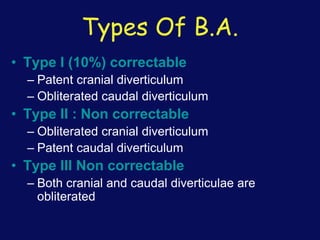
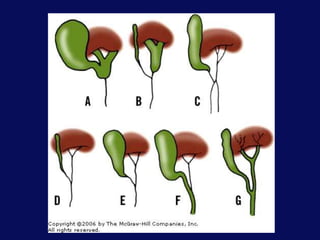
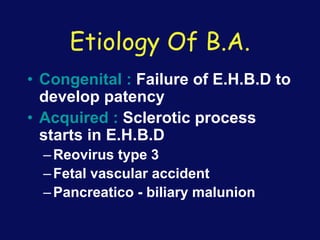
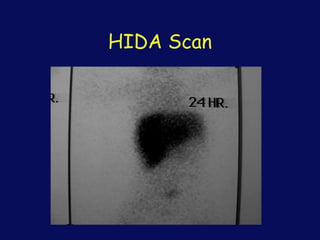
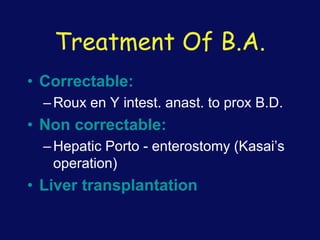
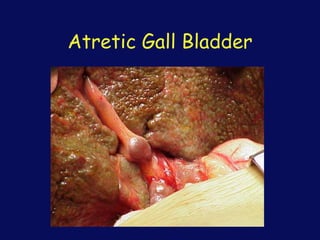
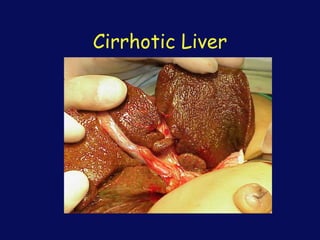
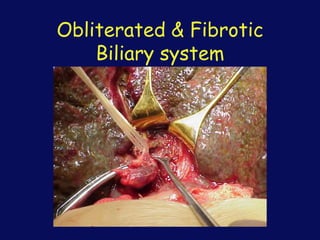
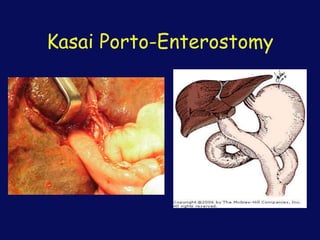
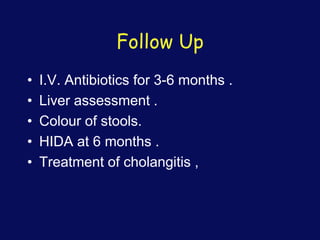
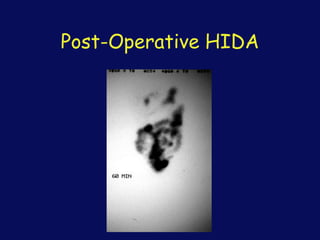
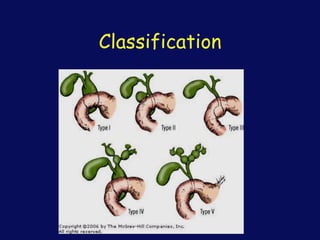
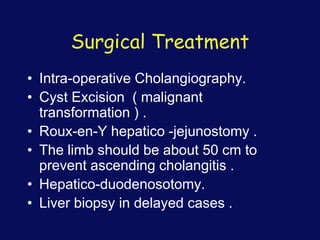
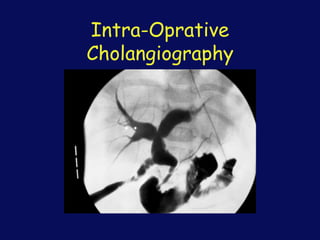
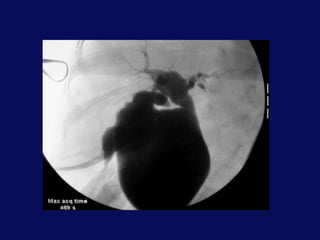
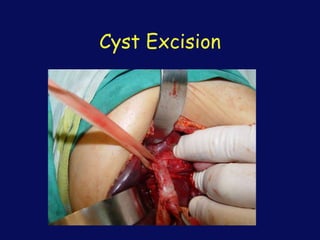
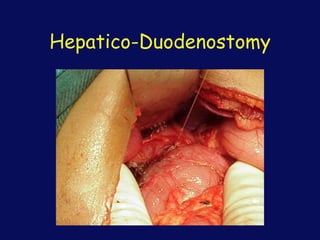
This document discusses the surgical anatomy of the liver and biliary tree. It begins with a description of liver embryology, including how the hepatic diverticulum and primordium form from the transverse septum and later differentiate into the mature liver and gallbladder. It then discusses the development of the biliary duct system and liver parenchyma. Key surgical landmarks, vasculature, variations, anomalies, and pathological conditions of the biliary tract are outlined, including biliary atresia and choledochal cysts. The classifications, diagnoses, and surgical treatments of these conditions are summarized.