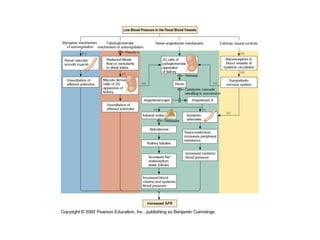
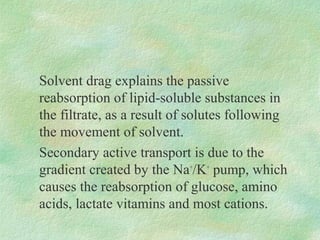
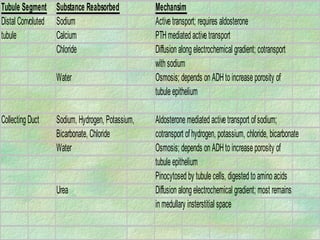
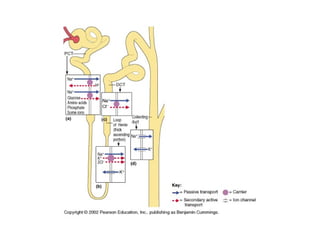
The document summarizes key concepts about excretion by the kidneys. It discusses glomerular filtration which forms filtrate from blood plasma, and the tubular reabsorption and secretion processes that modify the filtrate to form urine and remove wastes. Specifically, it describes the mechanisms of passive and active transport that allow reabsorption of useful solutes and water back into blood from the filtrate in different kidney tubule segments. The countercurrent mechanism and role of antidiuretic hormone in regulating urine concentration and volume are also summarized.