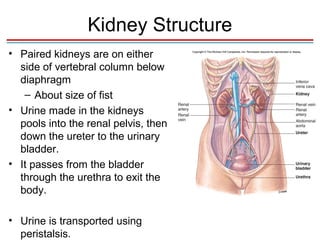
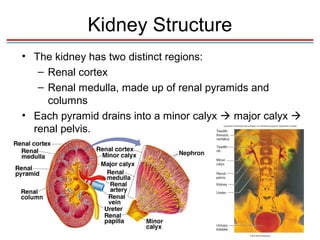
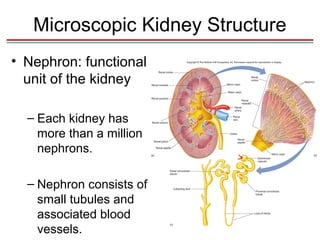
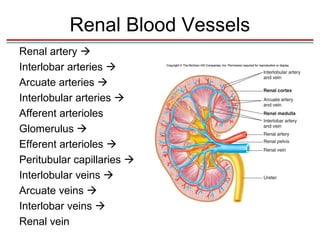
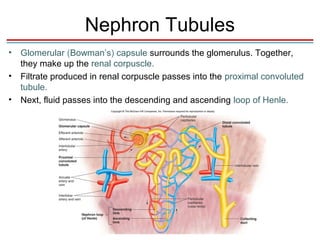
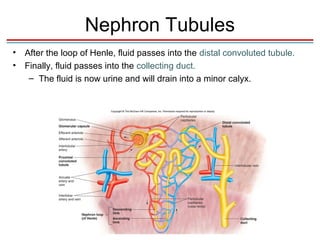
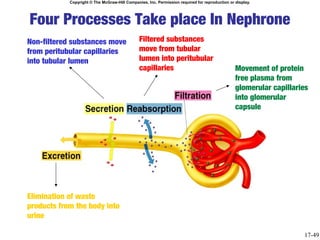
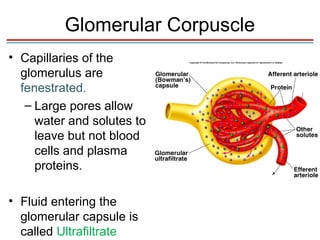
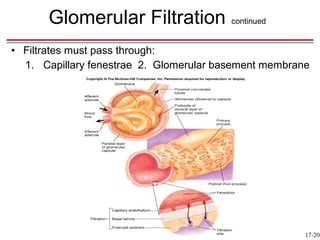
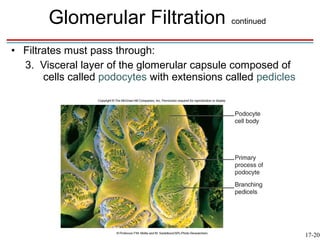
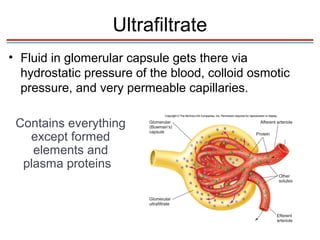
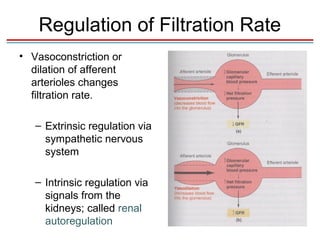
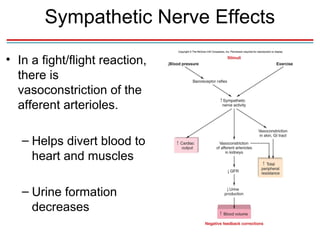
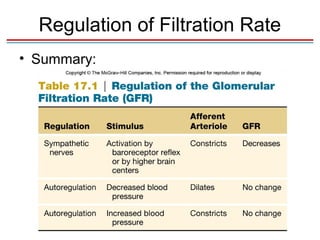
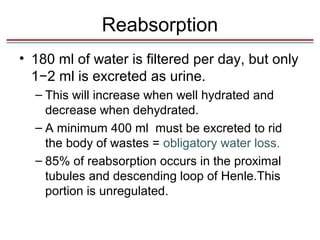
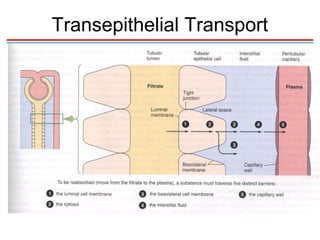
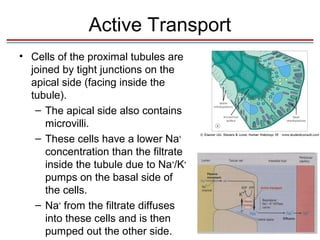
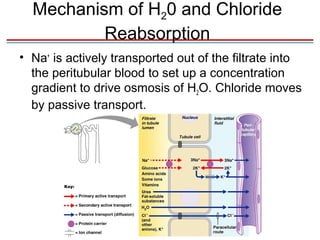
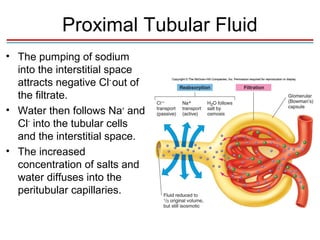
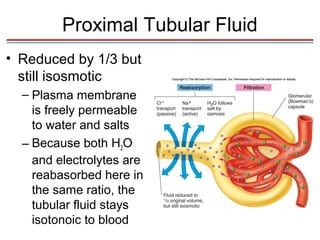
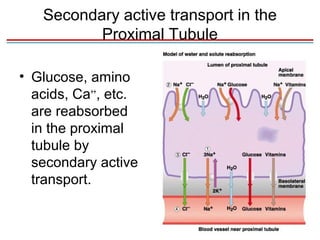
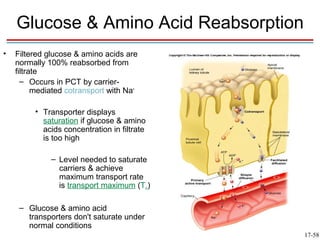
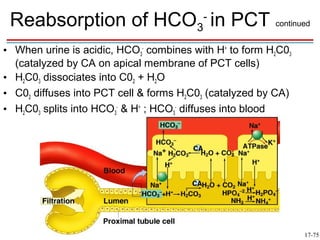
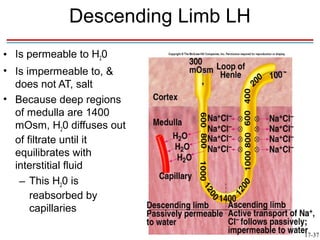
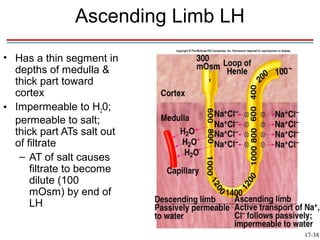
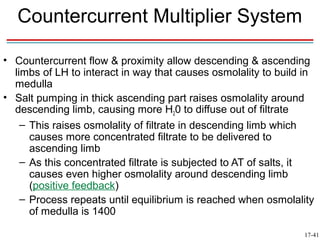
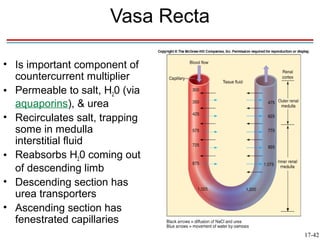
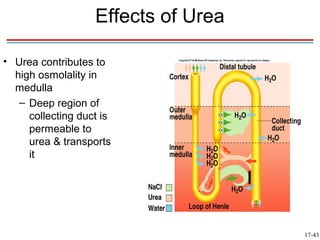
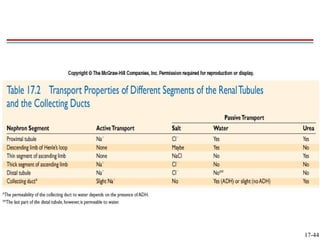
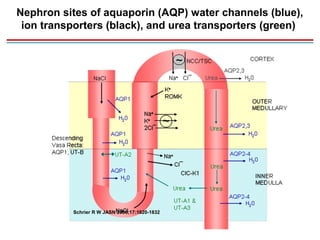
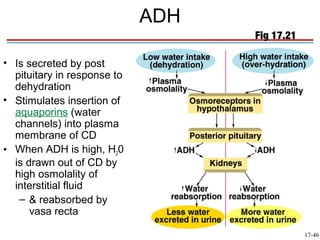
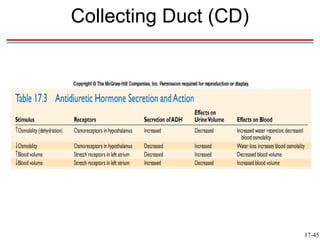
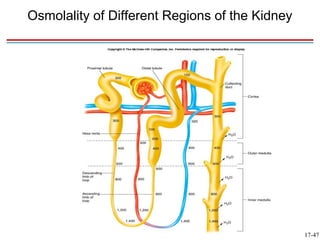
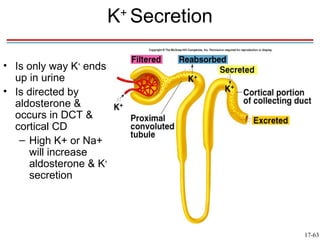
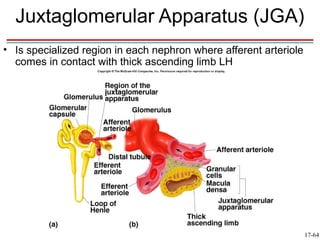
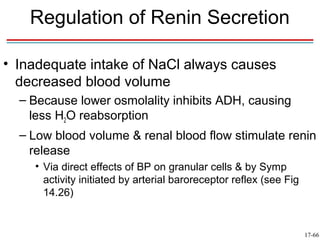
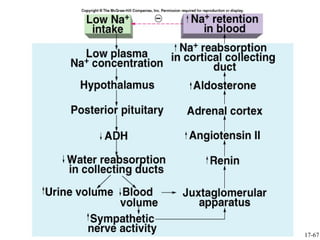
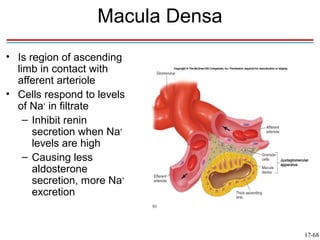
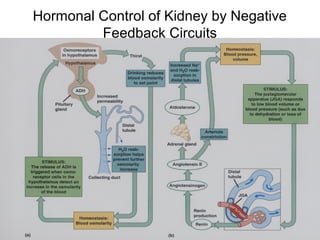
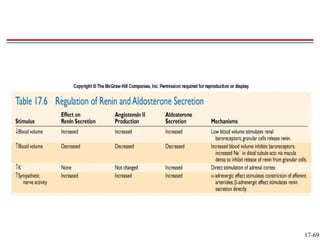
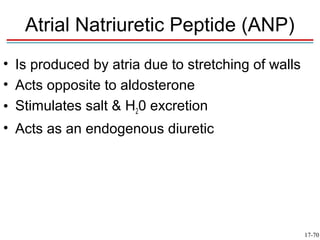
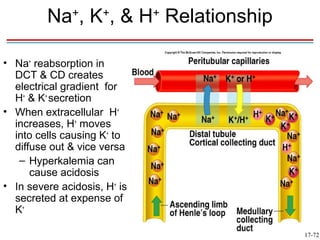
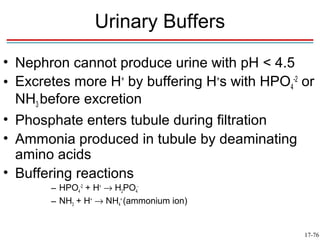
The document discusses the physiology of the kidneys, describing their role in maintaining homeostasis through functions like regulating water balance and electrolyte concentrations, as well as their internal structure including nephrons and the processes of glomerular filtration, reabsorption of water and salts, and production of urine. Key concepts covered include kidney anatomy, the roles of different kidney structures like the nephron and collecting duct, and physiological mechanisms involved in filtration, reabsorption, and regulation of fluids and electrolytes.