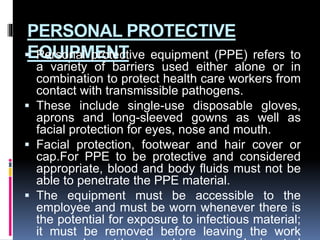
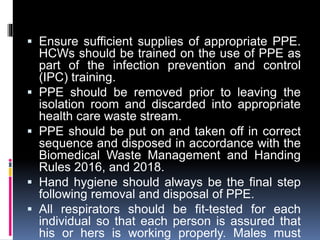
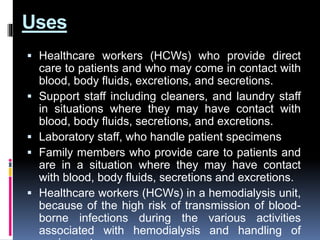
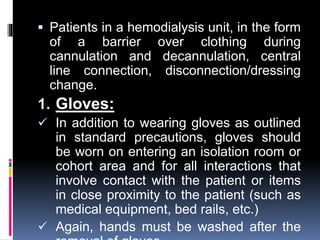
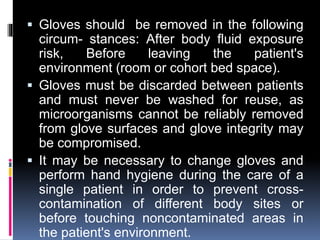
The document outlines CDC guidelines for infection prevention and control in healthcare settings, emphasizing the importance of PPE and proper practices to mitigate the risk of transmission of communicable diseases. It details the types of PPE required, including gloves, aprons, gowns, facial protection, and footwear, while also highlighting the necessity of hand hygiene and appropriate disposal of contaminated materials. Additionally, it underscores the need for training healthcare workers on proper PPE use and adherence to safety protocols to safeguard both staff and patients.