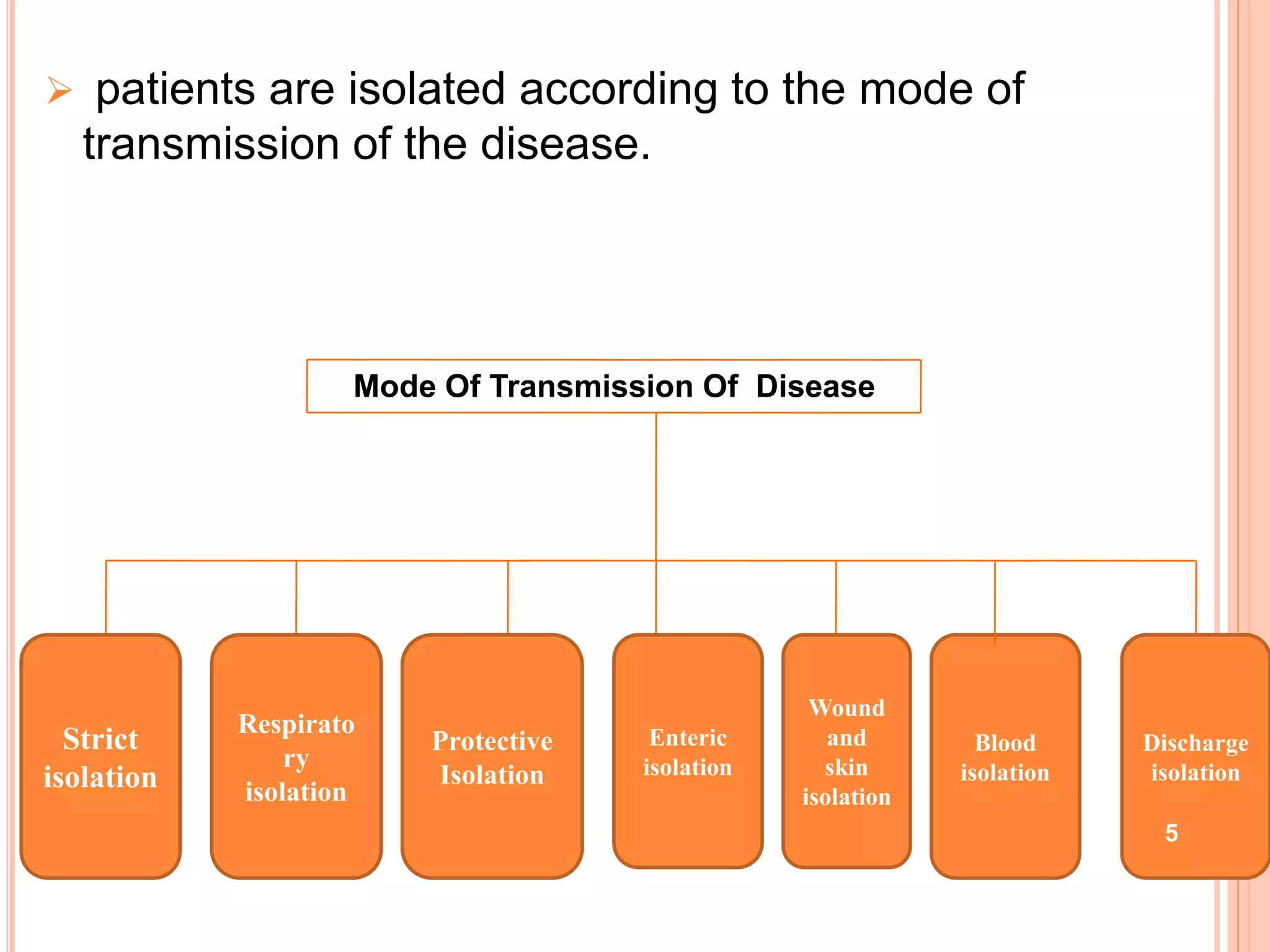
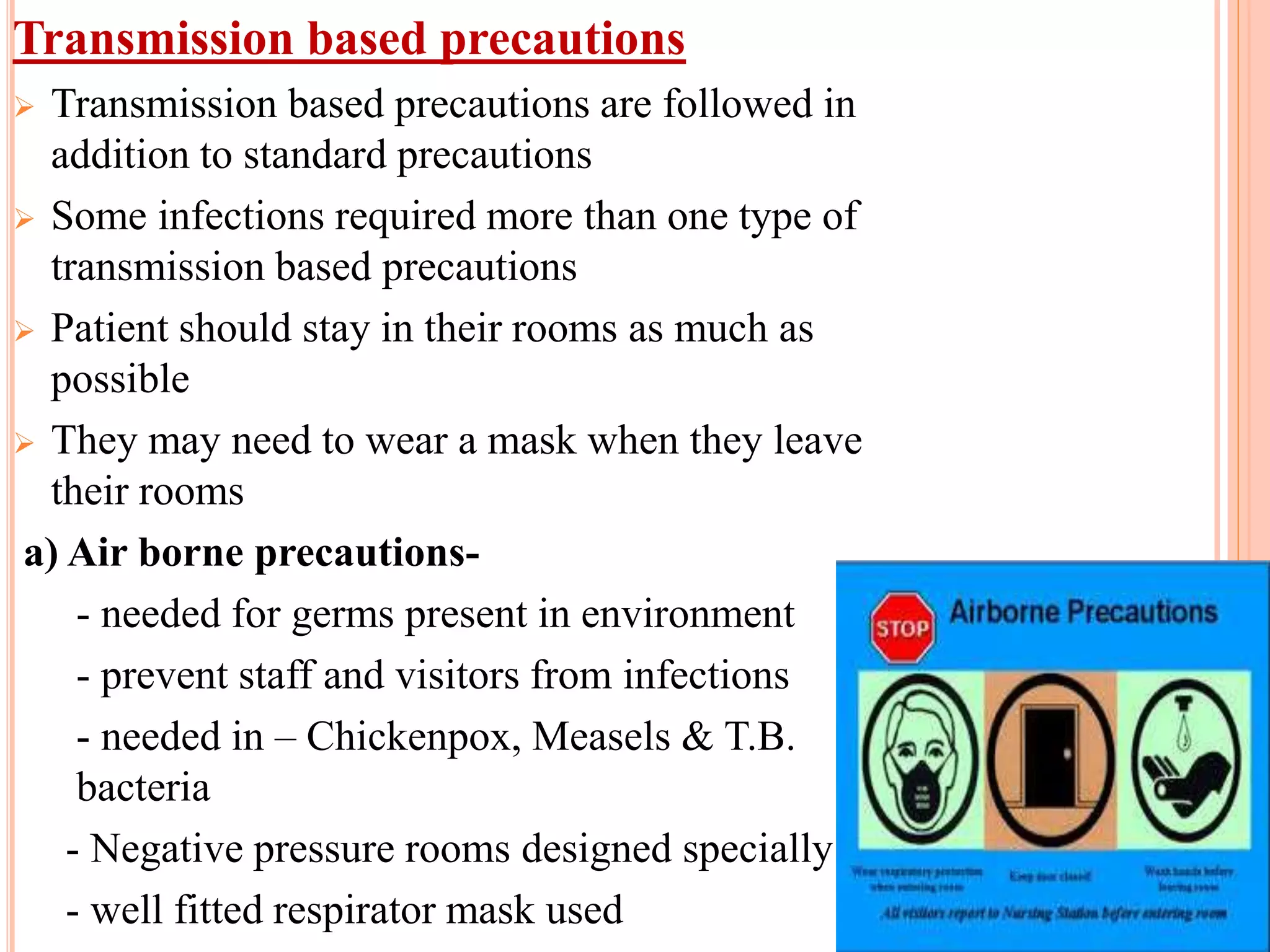
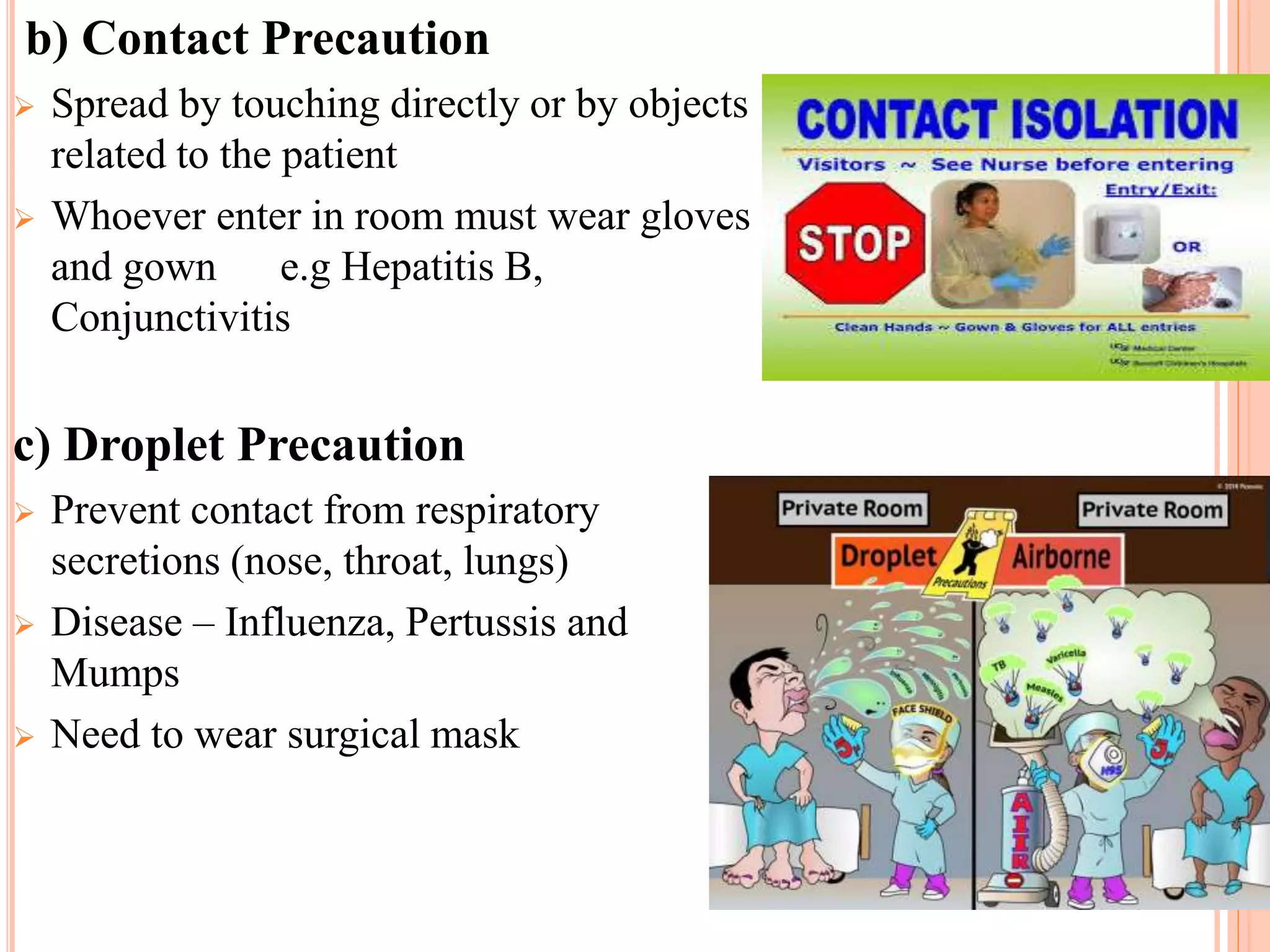
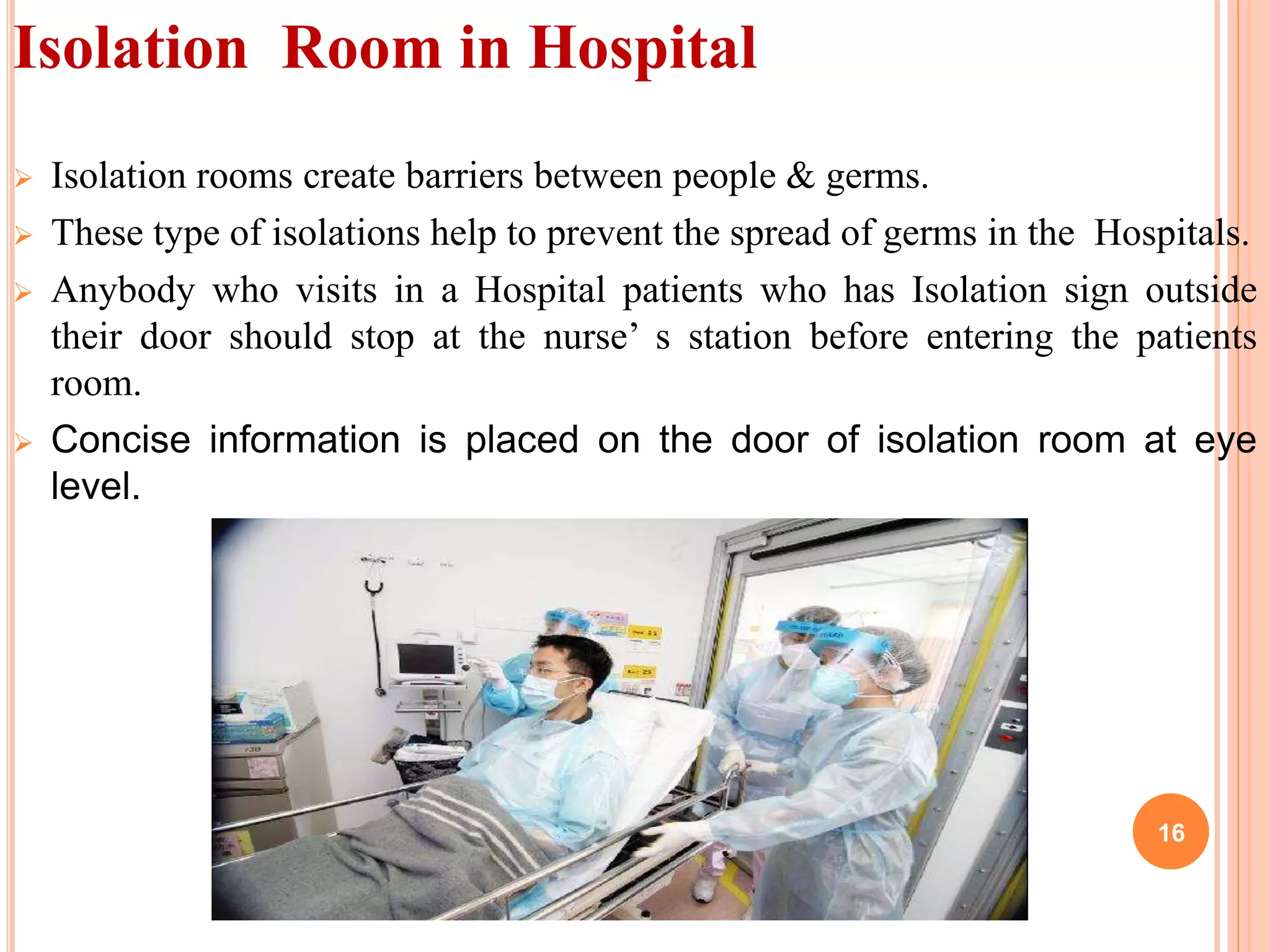
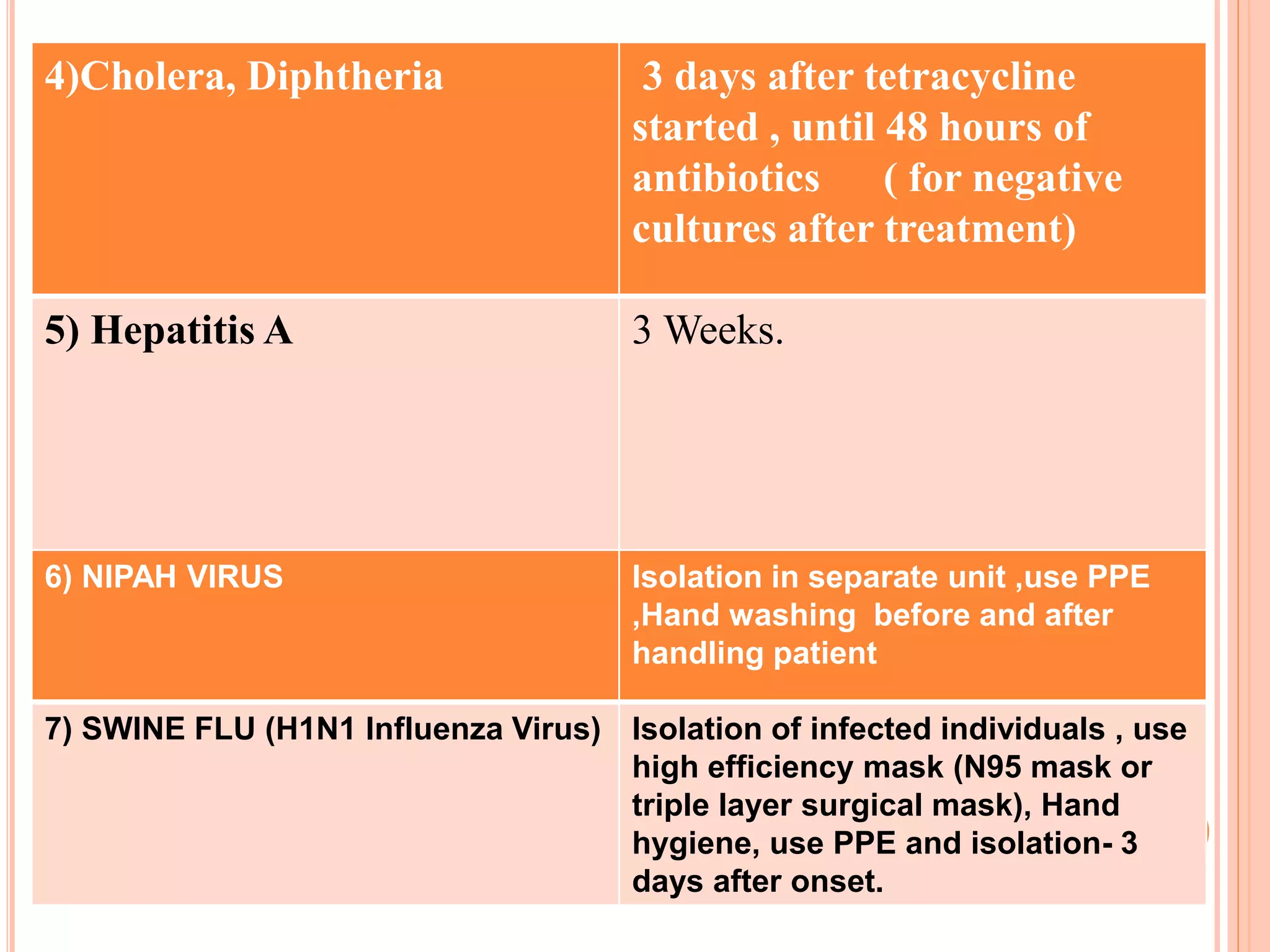
The document discusses isolation as a critical measure to control the spread of infectious diseases in healthcare settings, highlighting various types of isolation based on disease transmission modes. It outlines types of precautions to be taken, advantages and disadvantages of isolation, and specific protocols for different diseases. Additionally, it reflects on historical perspectives and concludes that while isolation is essential for public health, it may pose challenges for the isolated individual.