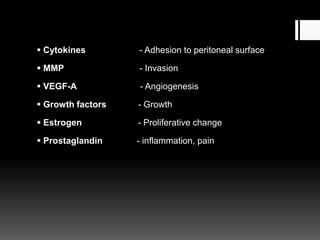
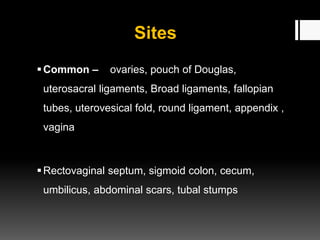
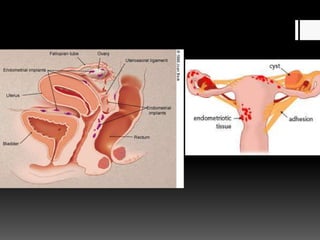
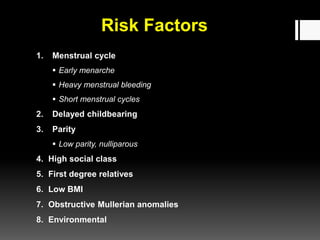
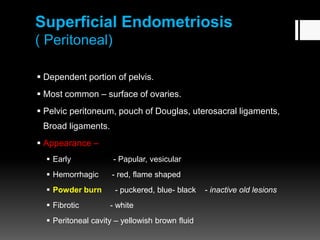
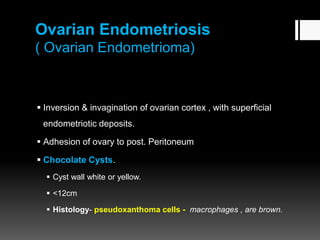
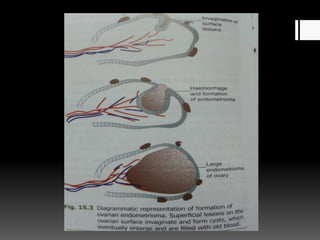
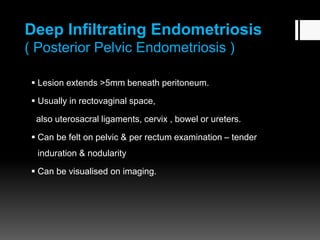
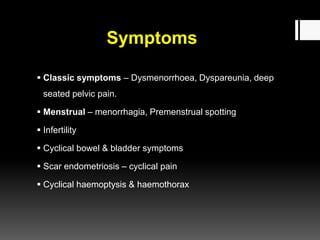
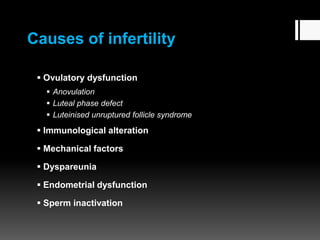
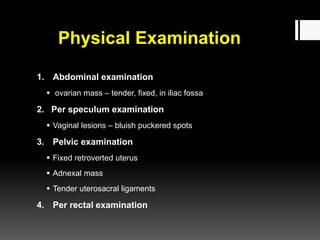
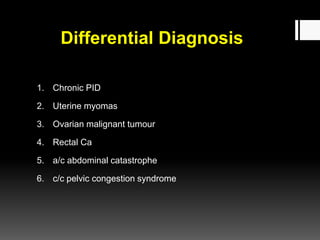
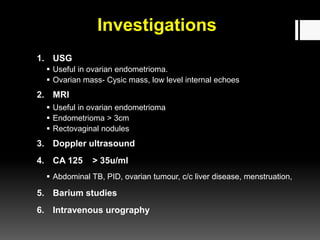
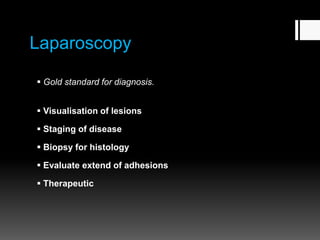
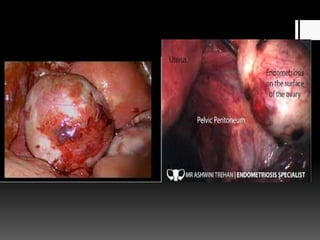
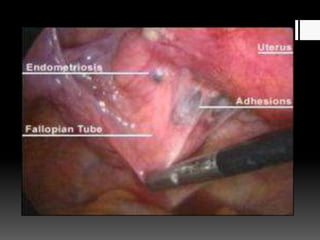
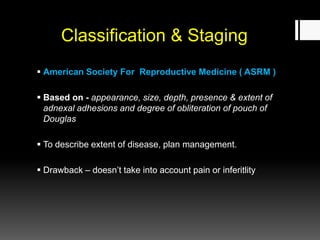
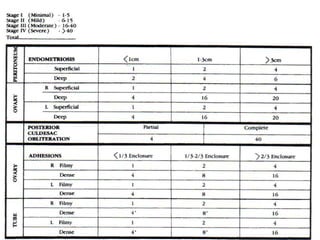
This document discusses endometriosis, a condition where endometrial tissue grows outside the uterus. It causes pain and infertility. The document covers the pathogenesis, risk factors, classification into superficial, ovarian, and deep infiltrating types based on location and severity. Symptoms include painful periods and sex. Diagnosis involves physical exam, ultrasound, MRI and laparoscopy. Staging uses the ASRM system from minimal to severe based on extent of disease and adhesions. Treatment aims to control symptoms and improve fertility.