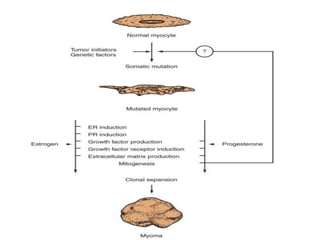
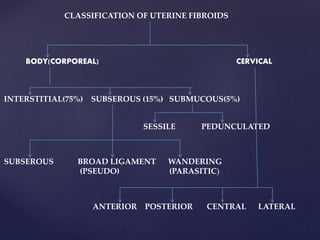
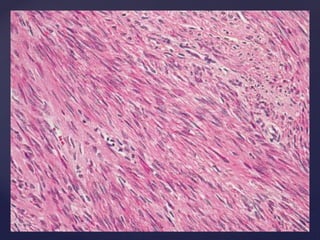
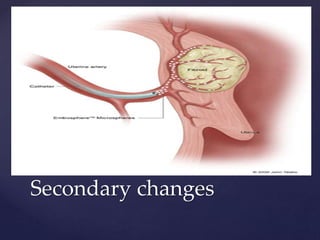
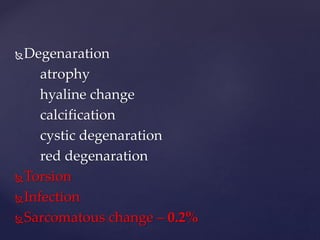
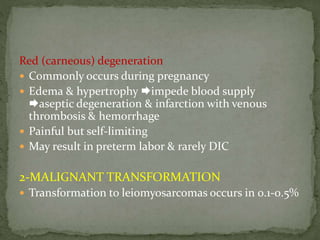
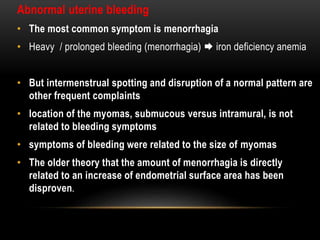
Fibroids are benign tumors that occur in the uterus and are quite common, affecting approximately 25% of women. They develop from muscle cells in the uterus and can vary in size and location. The most common symptoms are abnormal uterine bleeding and pain. Clinical examination often reveals an enlarged, irregular uterus, and imaging tests may be used to further evaluate the size and location of any fibroids present. While usually asymptomatic, fibroids can sometimes cause complications during pregnancy like miscarriage or preterm labor, especially if they are located inside the uterine cavity.