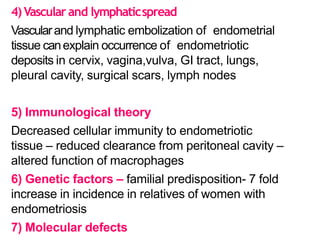
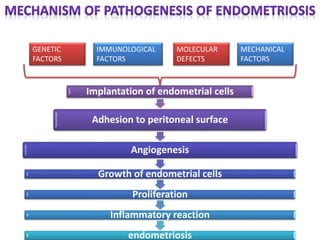
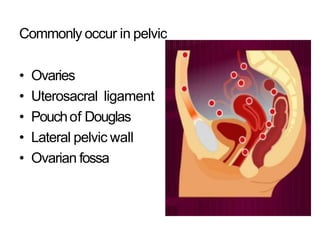
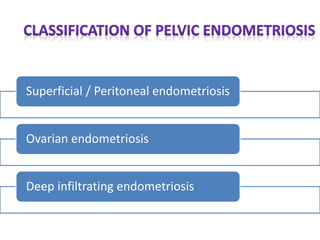
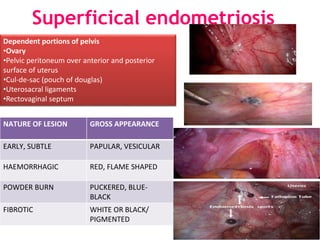
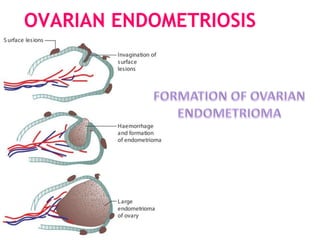
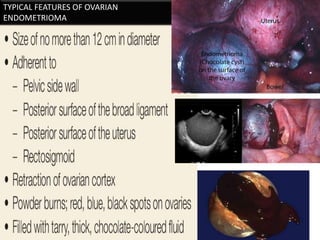
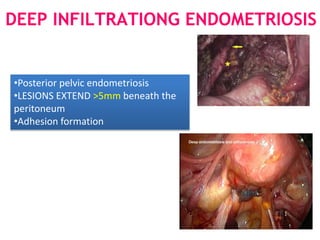
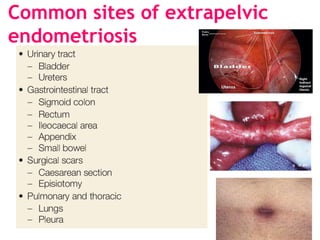
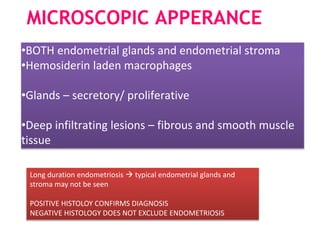
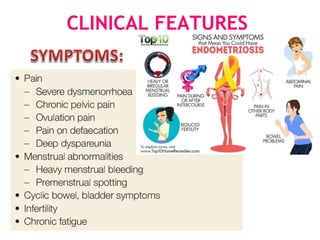
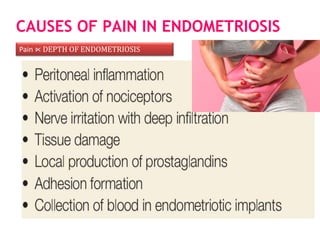
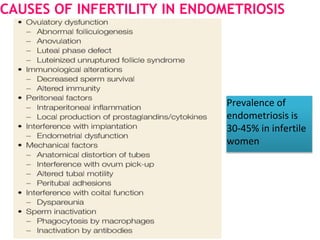
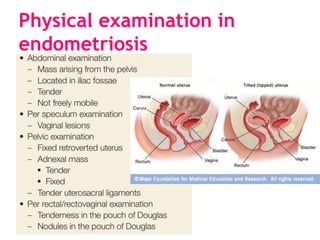
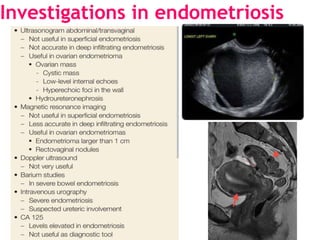
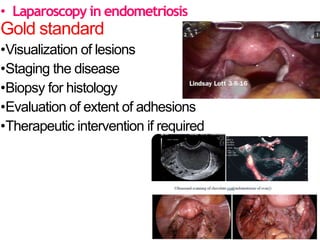
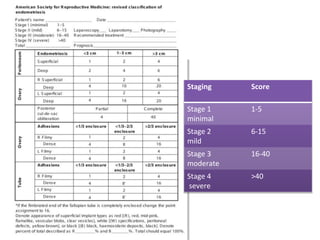
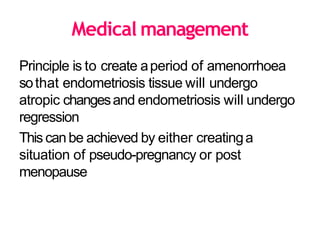
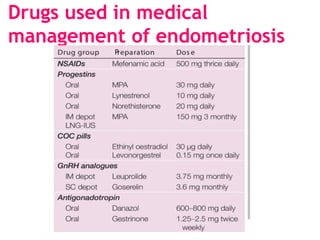
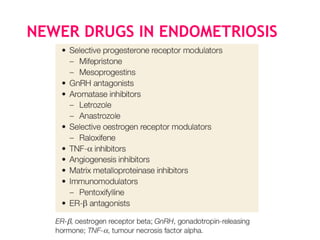
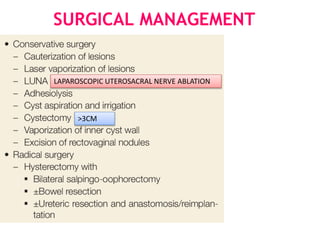
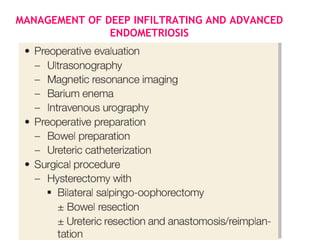
Endometriosis is a common benign gynecological condition defined by the presence of endometrial glands and stroma outside the uterus. It has a prevalence of 8-10% in reproductive aged women. Risk factors include early menarche, heavy periods, delayed childbirth, nulliparity, and family history. The exact cause is unknown but theories include retrograde menstruation implanting cells, coelomic metaplasia, and lymphatic/vascular spread. Common sites of lesions are the ovaries, pouch of Douglas, and uterosacral ligaments. Treatment involves laparoscopy for diagnosis and staging, with medical management using hormonal therapies or surgery for deep infiltrating disease.