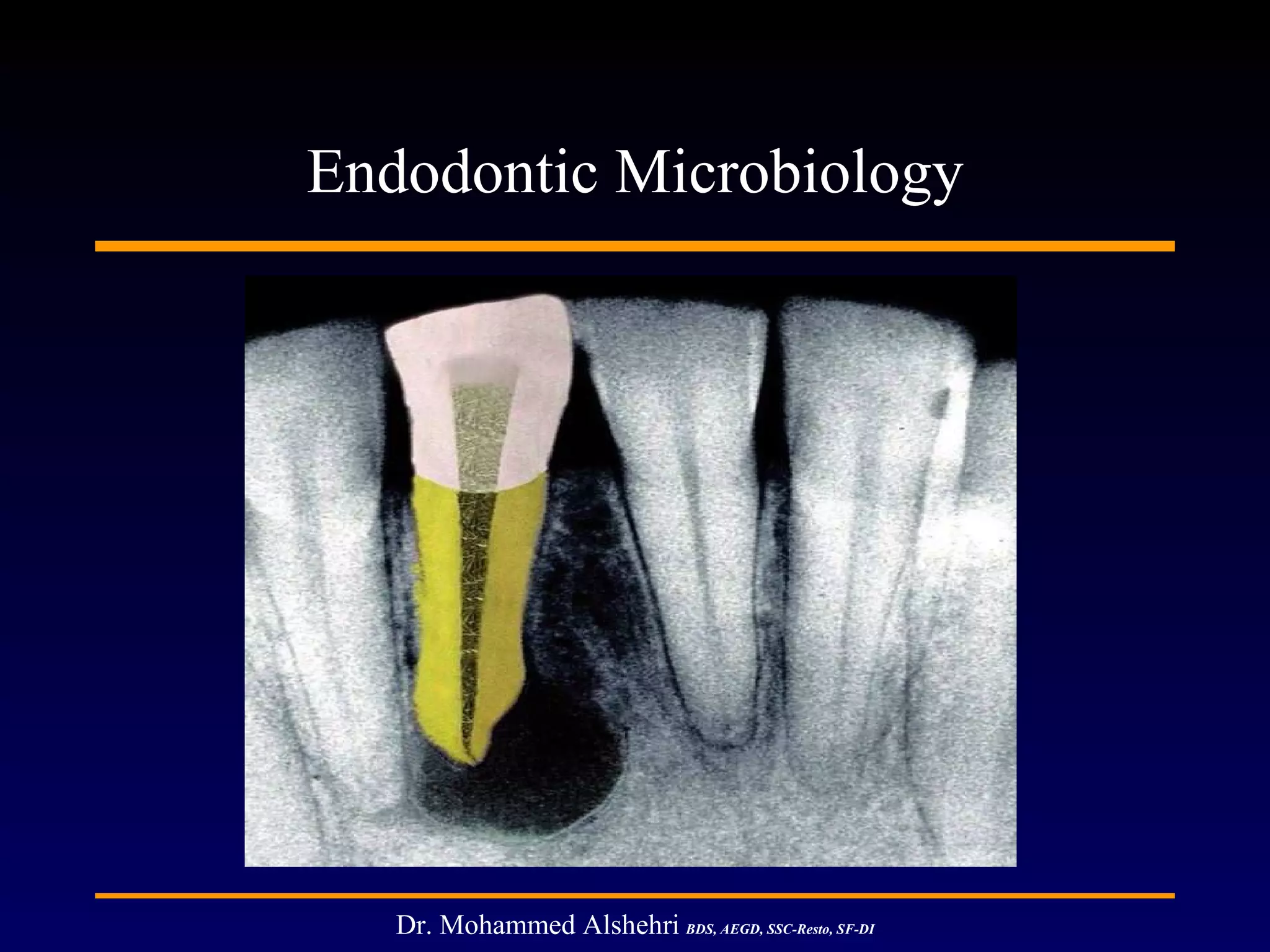
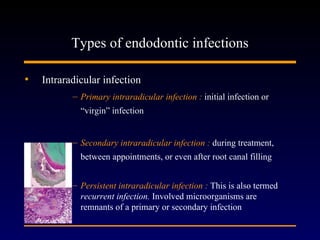
1) Apical periodontitis is caused by microbial infection of the root canal system, usually after pulp necrosis. Bacteria are the primary cause, though fungi and archaea have also been implicated.
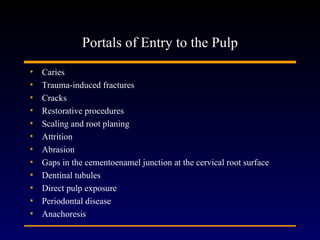
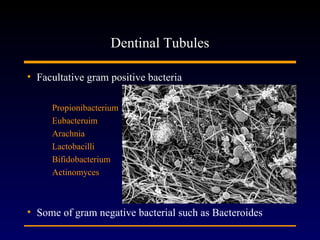
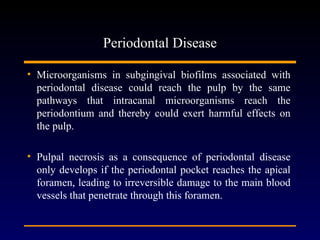
2) Bacteria enter the root canal system through caries, cracks, restorative procedures, or periodontal disease. They can also travel through dentinal tubules or directly expose the pulp.
3) Successful endodontic treatment aims to prevent or resolve apical periodontitis by thoroughly debriding and disinfecting the root canal system.