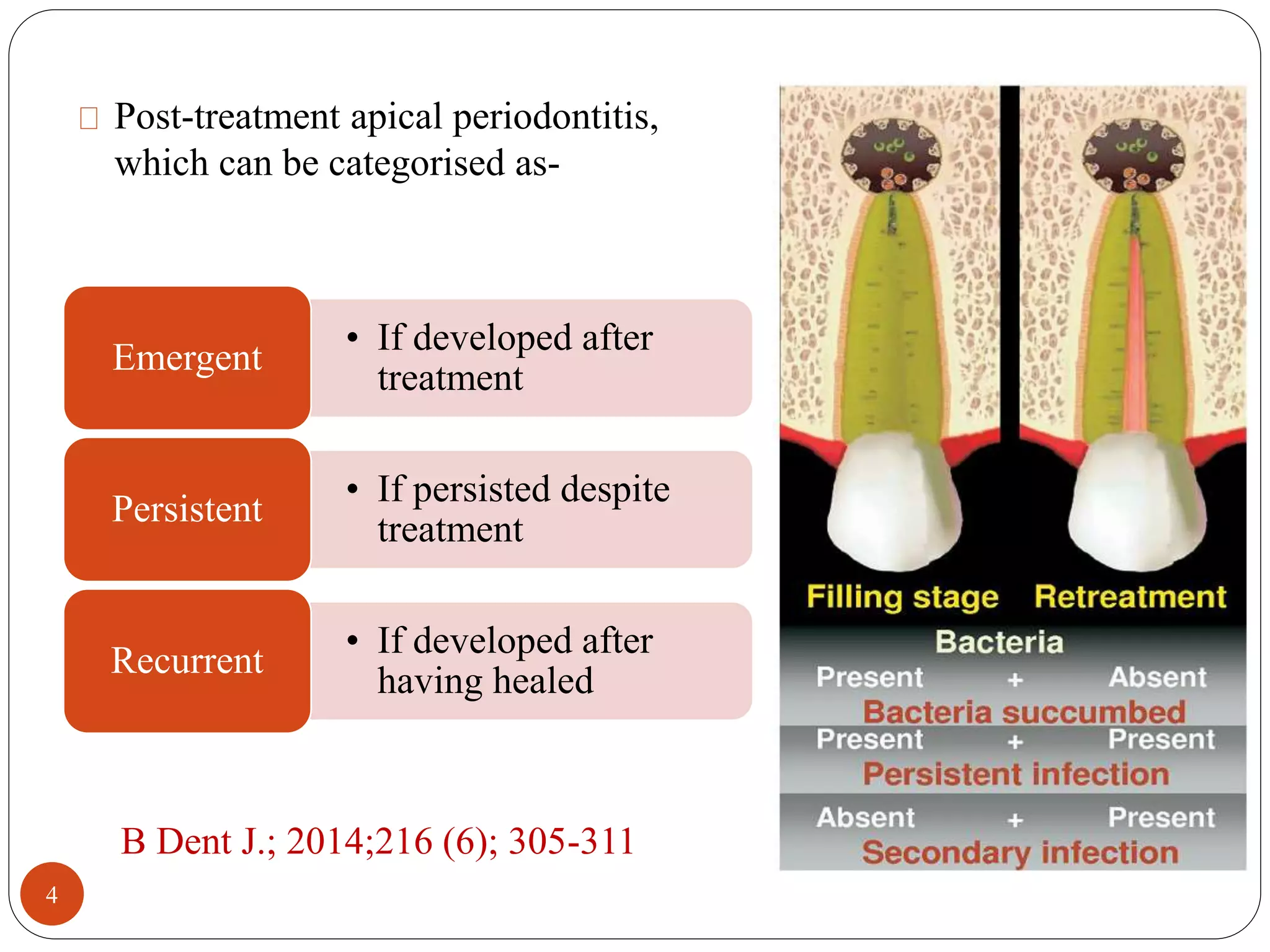
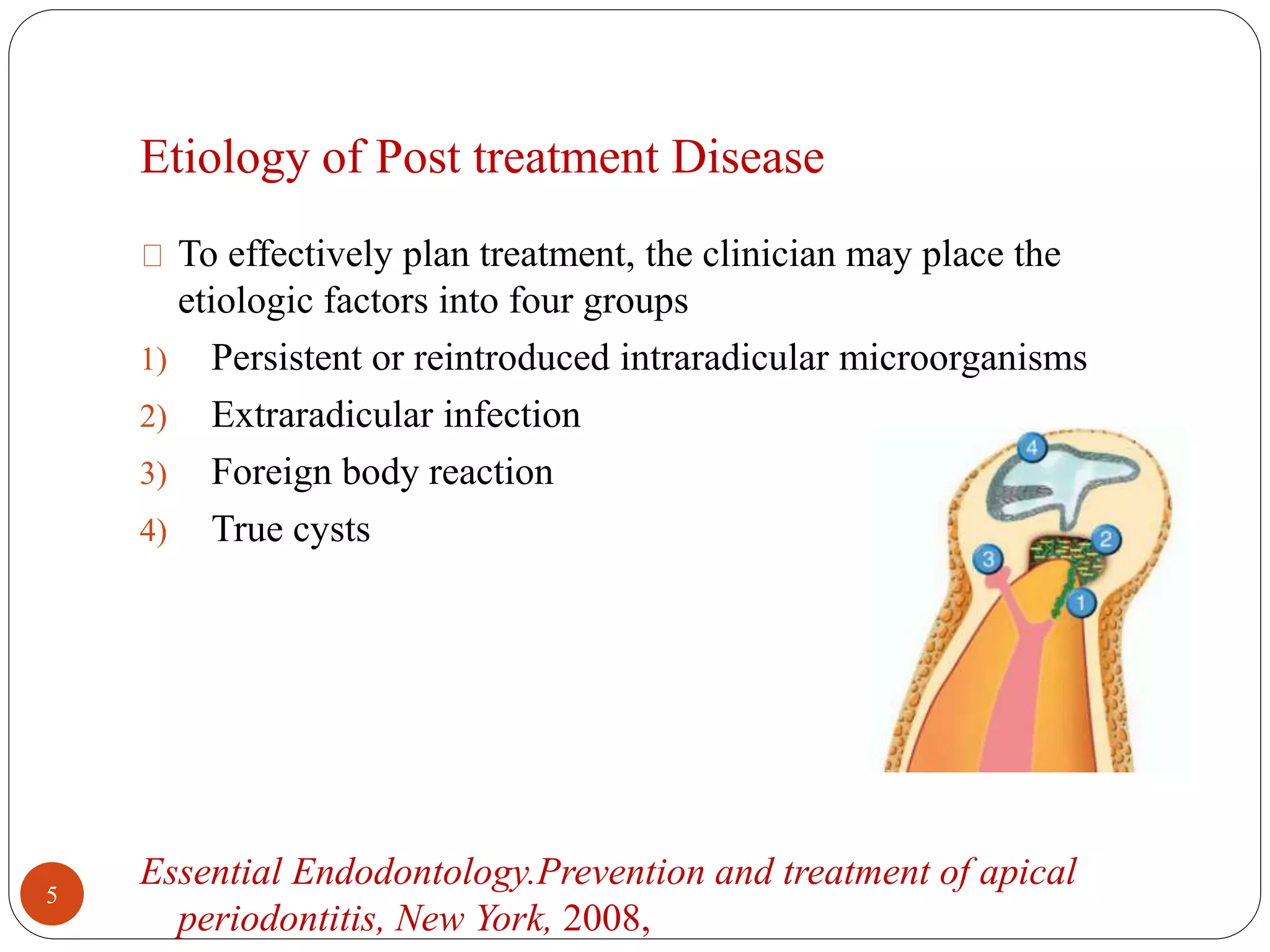
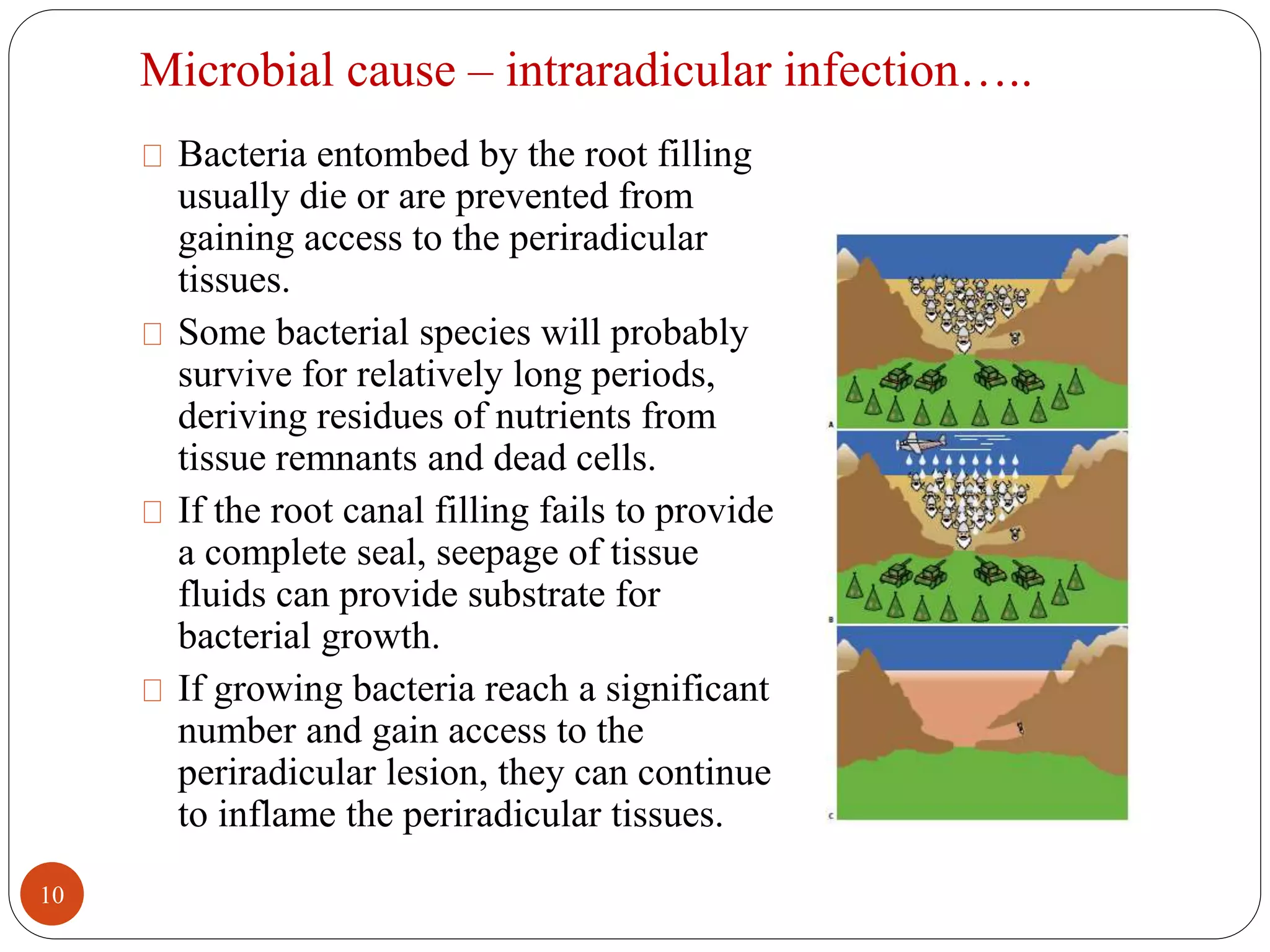
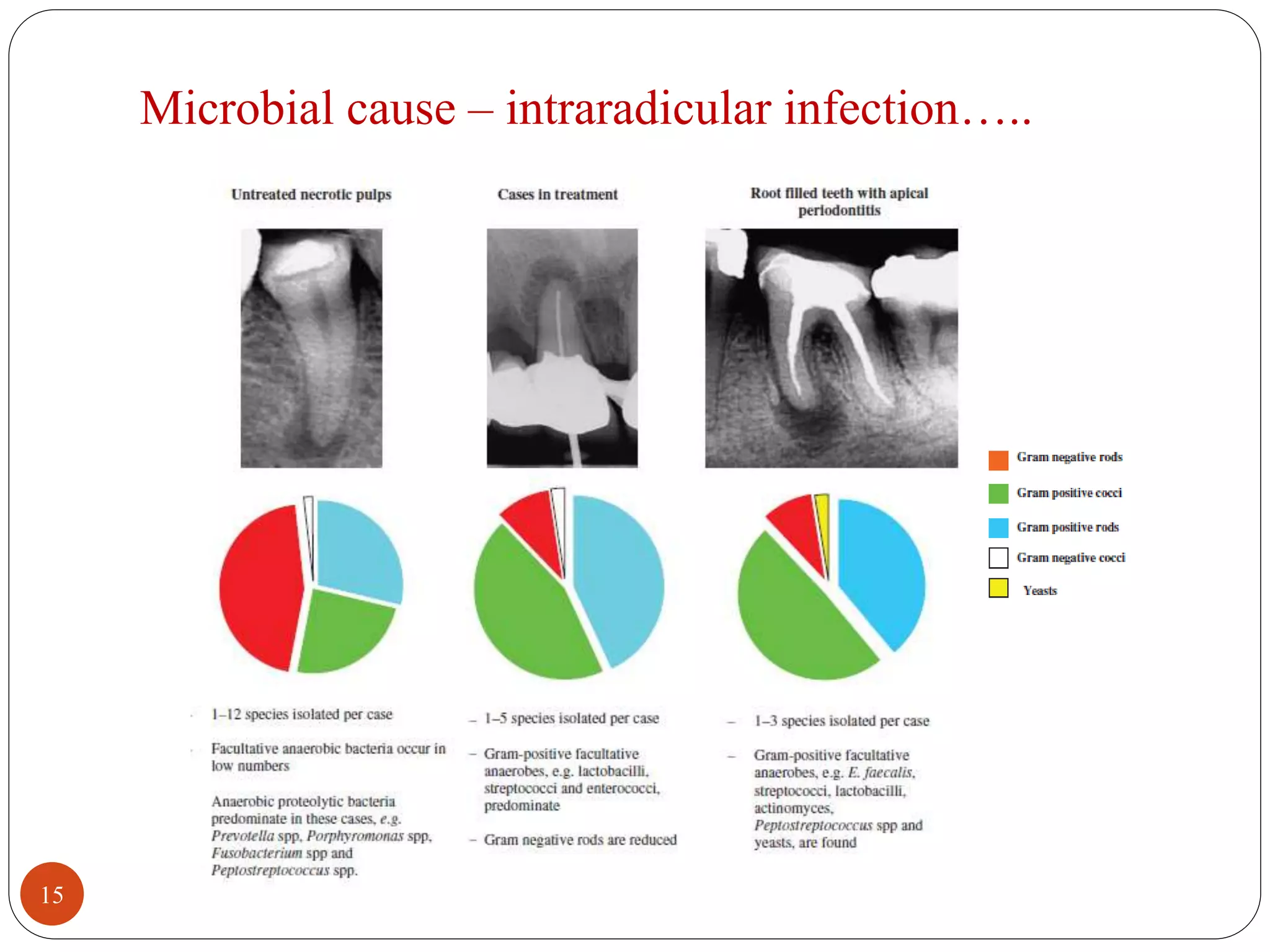
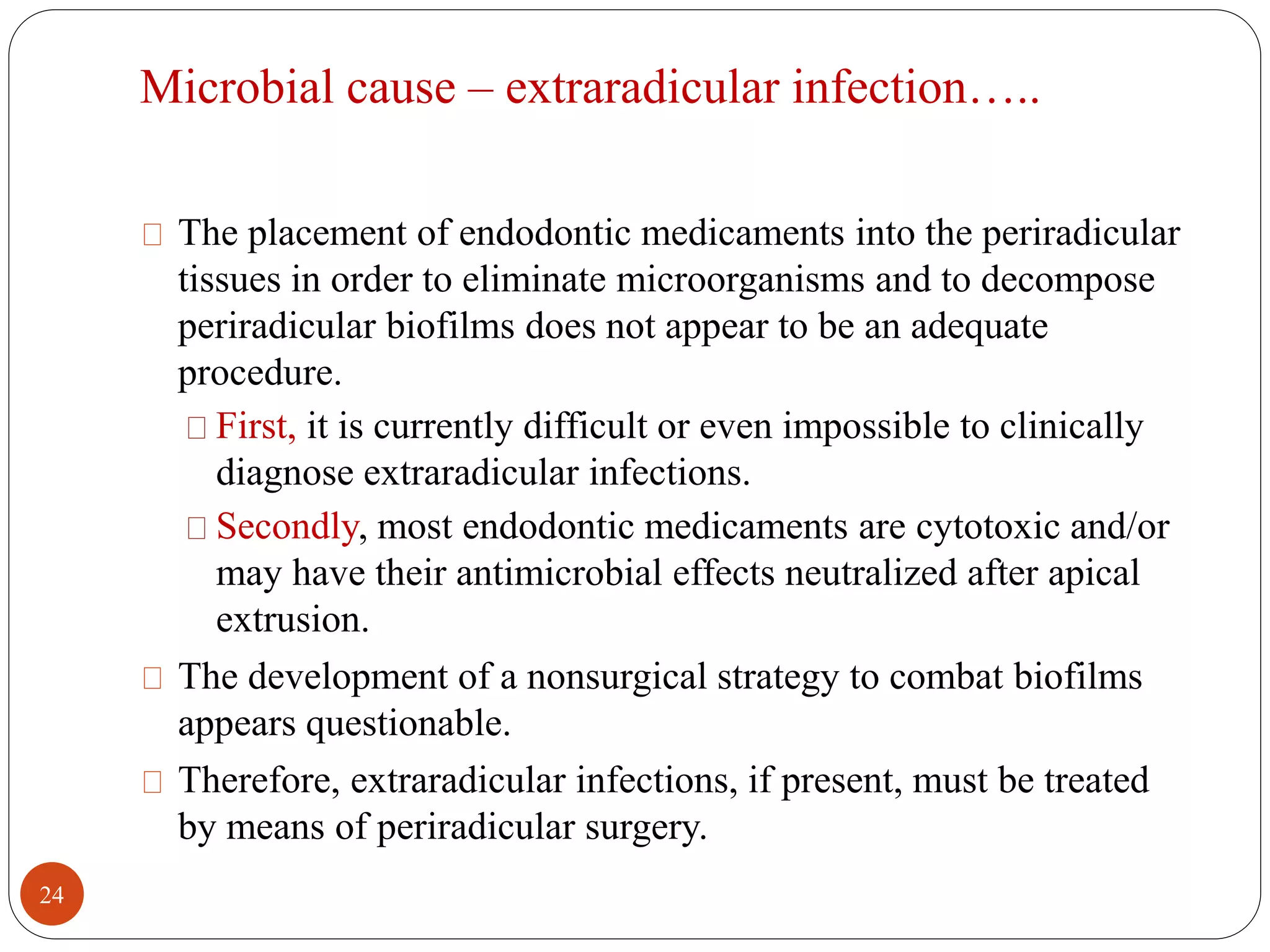
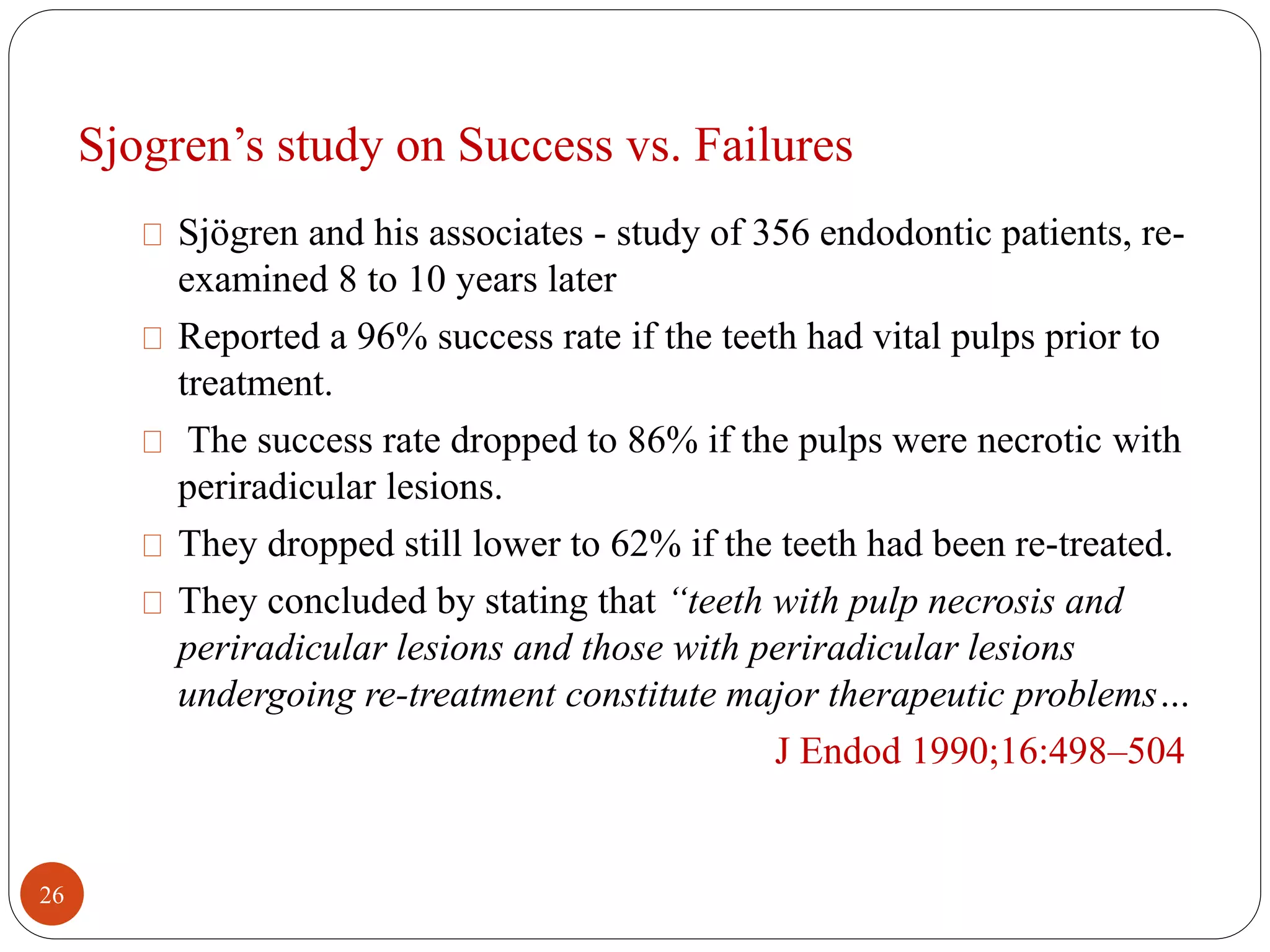
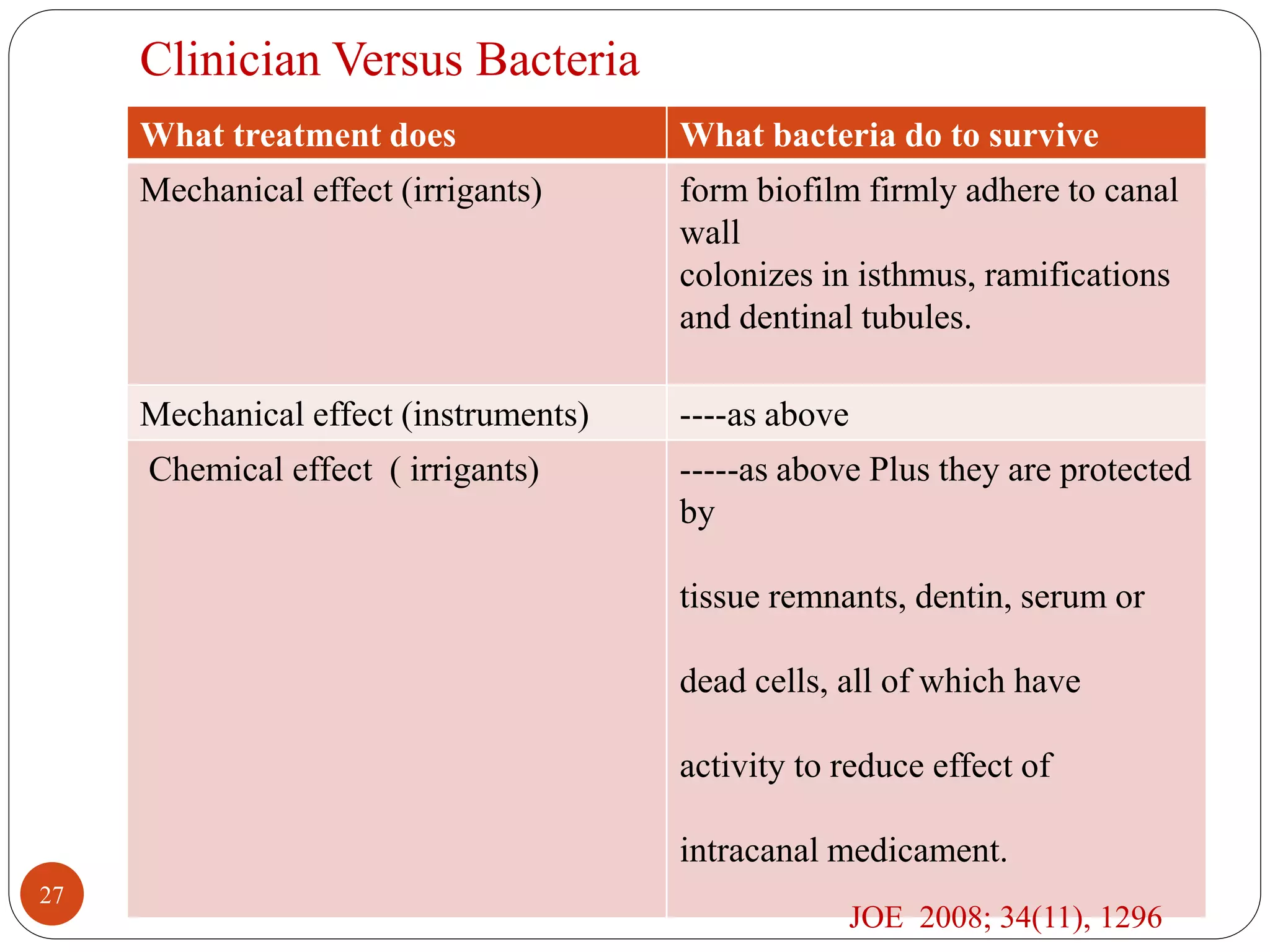
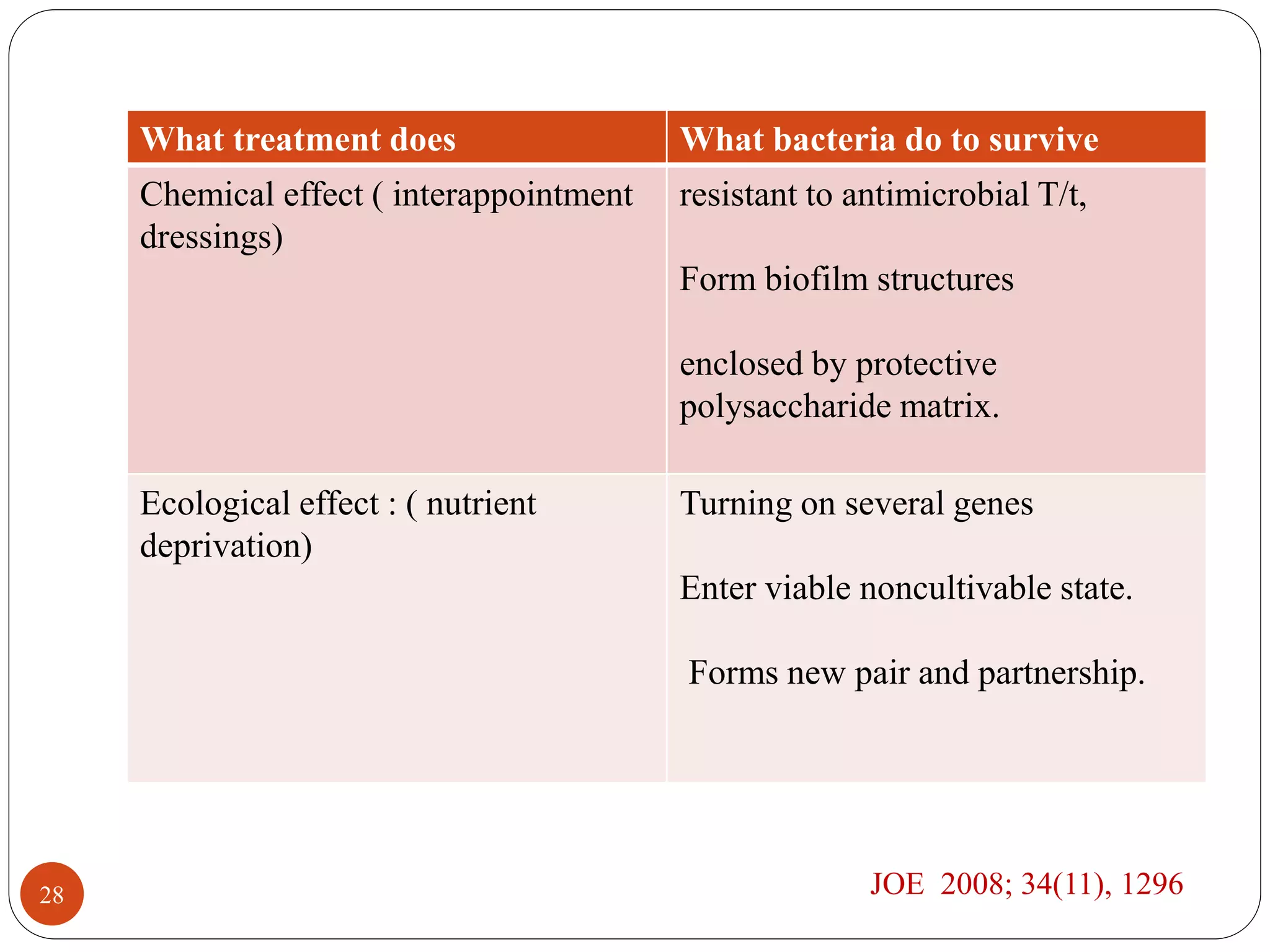
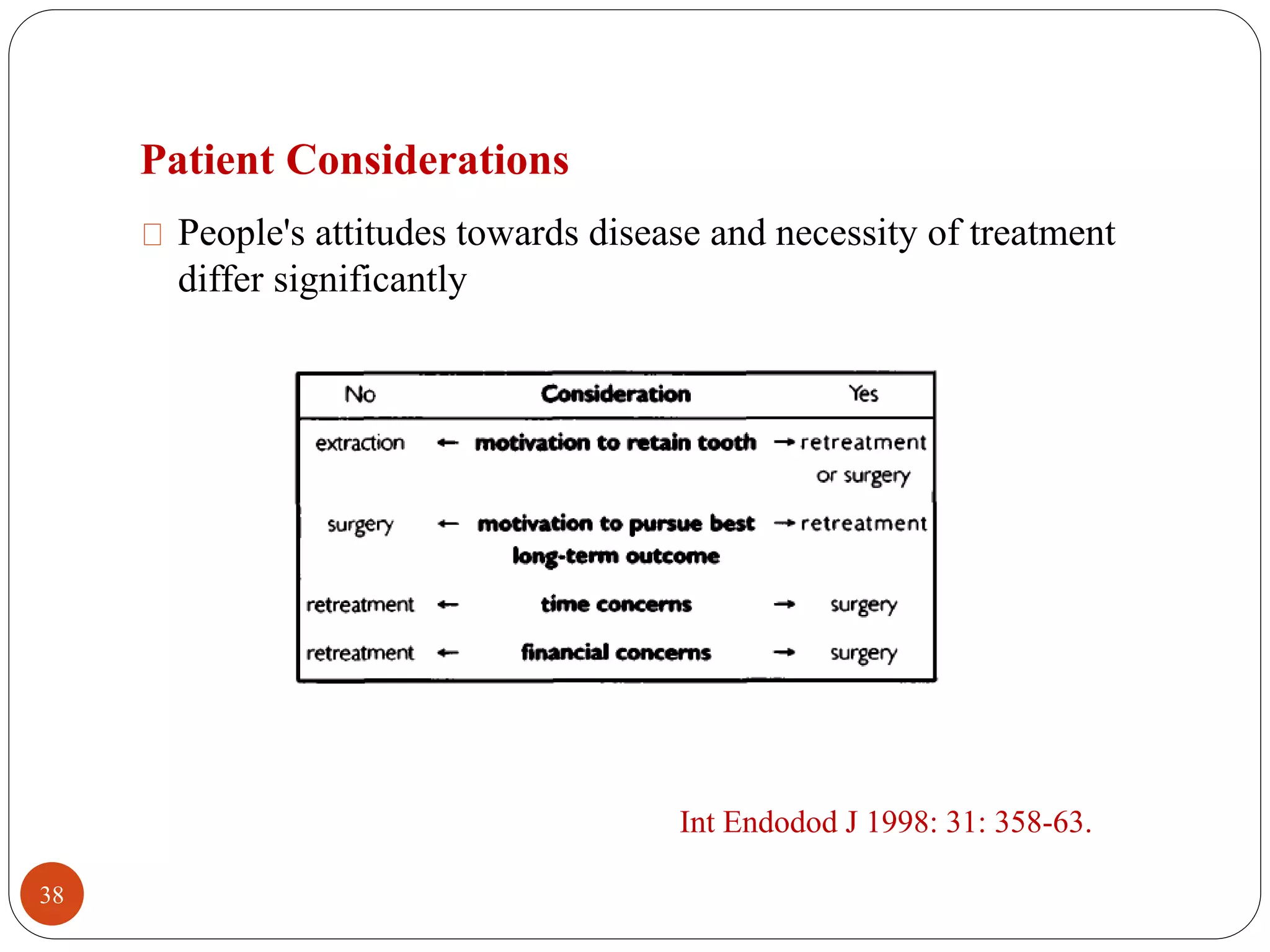
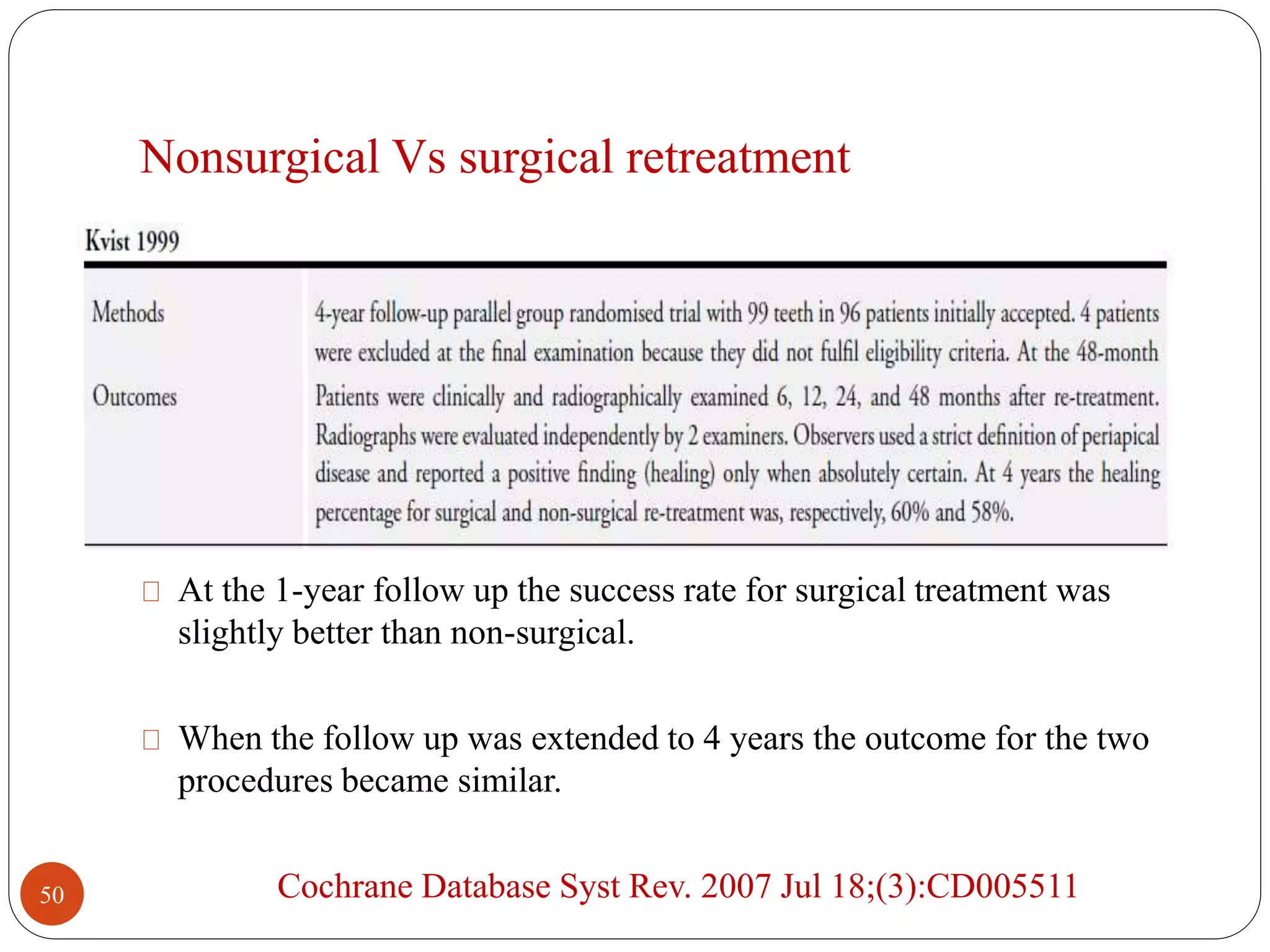
The document discusses causes and management of post-treatment endodontic disease. It identifies several potential causes of post-treatment apical periodontitis including persistent or reintroduced intraradicular microorganisms, extraradicular infection, foreign body reaction, and true cysts. Persistent intraradicular infections are the major cause, with bacteria able to survive through biofilm formation, entering dormant states, and activating stress response genes. Extraradicular infections may also develop through biofilm formation on root surfaces. While some case reports have suggested non-microbial causes, microbes are often difficult to rule out as a contributing factor.