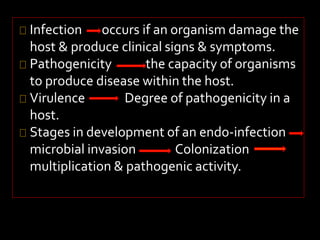
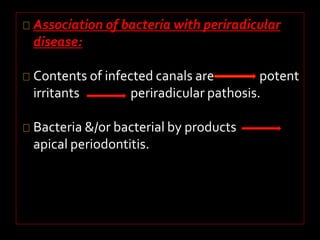
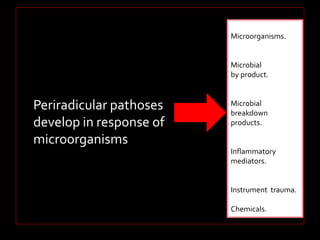
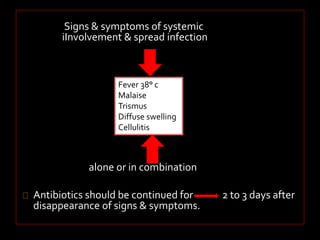
- Infection occurs when microorganisms invade tissues and produce clinical signs and symptoms of disease.
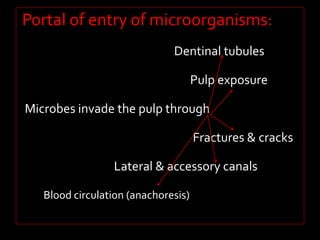
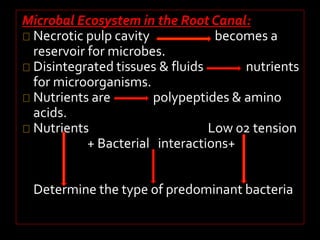
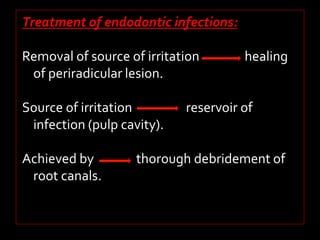
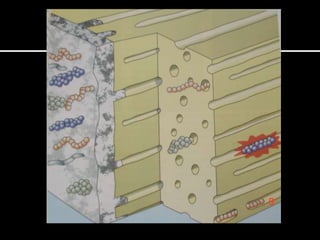
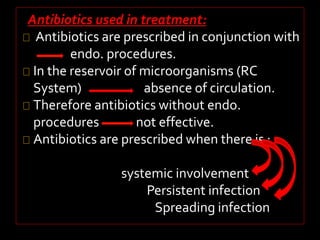
- The root canal system can become infected through dentinal tubules, lateral canals, or pulp exposure providing a reservoir for microbial growth.
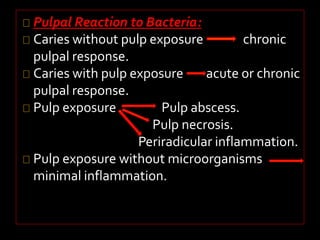
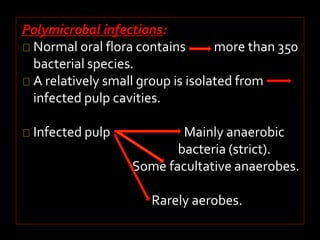
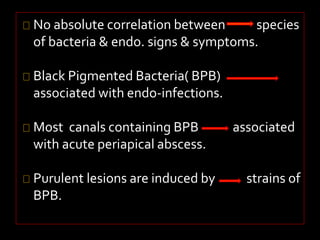
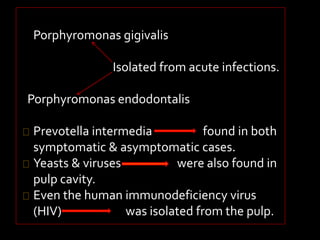
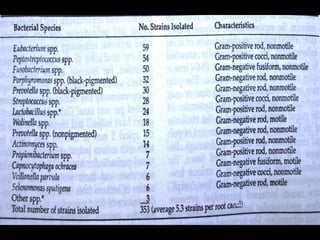
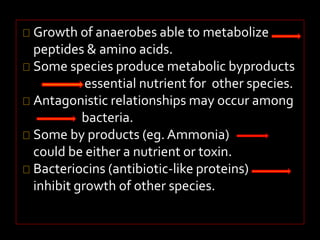
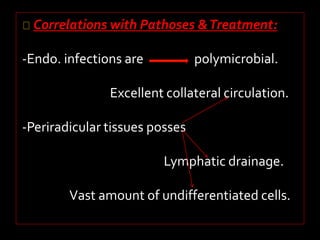
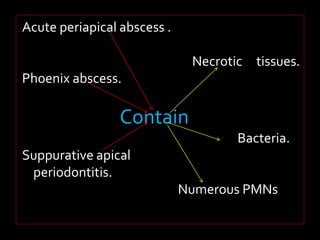
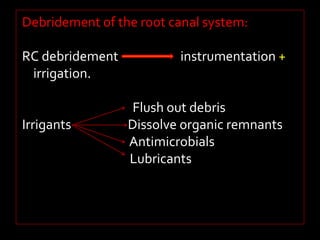
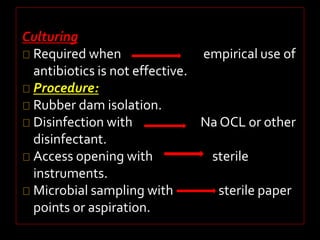
- Root canal infections are usually polymicrobial, involving both anaerobic and facultative bacteria, and treatment aims to disrupt the microbial ecosystem through debridement and disinfection to eliminate infection and allow healing of surrounding tissues.