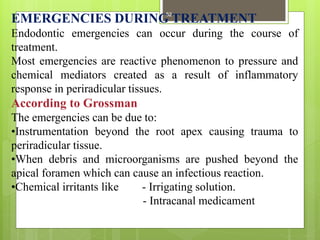
Endodontic emergencies are urgent dental situations primarily involving pain and swelling due to pulpo-periapical pathosis, requiring immediate diagnosis and treatment. These emergencies often arise due to stress or aggravation in patients and can include conditions such as acute pulpitis, alveolar abscess, and tooth fractures. Effective management relies on rapid diagnosis through patient history, clinical examination, and appropriate treatment interventions for pain relief and infection control.
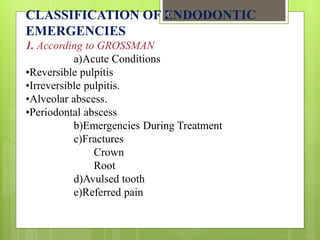
![2. According to GUTTMAN
I] TREATMENT OF VITAL PULP
Acute reversible pulpitis
Hypersensitive dentin.
Recurrent decay.
Recent restoration.
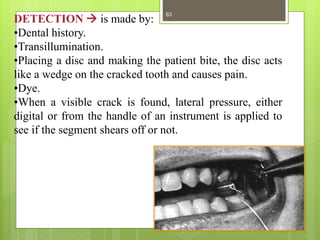
Cracked tooth syndrome.
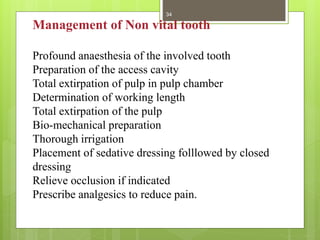
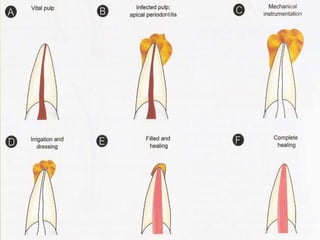
II] TREATMENT OF NON-VITAL PULP
Acute apical periodontitis.
Necrotic pulp.
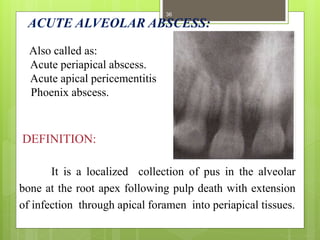
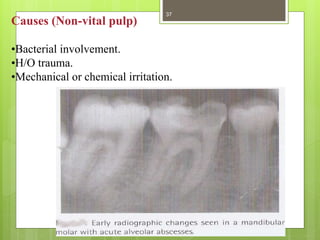
Acute alveolar abscess.
Phoenix abscess.
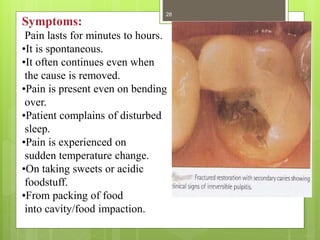
Acute irreversible pulpitis
- Localized.
- Non-localized
9](https://image.slidesharecdn.com/endodonticemergenciesfinal-151010115341-lva1-app6892/85/Endodontic-emergencies-9-320.jpg)
![III] ESTHETIC EMERGENCY
•Fracture of crown.
•Fracture of root.
•Avulsed tooth.
3. According to WALTON
(A)Pretreatment emergencies.
(B)Interappointment emergencies.
(C)Post-obturation emergencies
10](https://image.slidesharecdn.com/endodonticemergenciesfinal-151010115341-lva1-app6892/85/Endodontic-emergencies-10-320.jpg)
![ACUTE REVERSIBLE PULPITIS:-[Hyperemia]
DEFINITION:
It is a mild to moderate
inflammatory condition of the
pulp caused by noxious
stimuli in which the pulp is
capable of returning to the uninflamed state
following removal of the stimulus
20](https://image.slidesharecdn.com/endodonticemergenciesfinal-151010115341-lva1-app6892/85/Endodontic-emergencies-20-320.jpg)
![Acute Alveolar Abscess
Patient may present with no swelling,
with intra oral sinus OR
with swelling [facial asymmetry ]
45](https://image.slidesharecdn.com/endodonticemergenciesfinal-151010115341-lva1-app6892/85/Endodontic-emergencies-45-320.jpg)
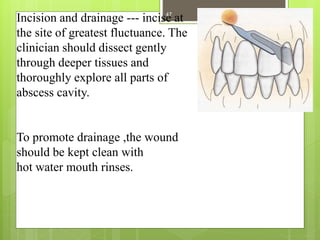
![WITH SWELLING:-
3 ways to resolve it:
1. Establish drainage through root canal
2. Establish drainage by incising a fluctuant swelling [if the
swelling is hard ,rinse it 3-5 mins with hot saline]
3. Antibiotics
use of antibiotics is regarded as an aid to drainage .
46](https://image.slidesharecdn.com/endodonticemergenciesfinal-151010115341-lva1-app6892/85/Endodontic-emergencies-46-320.jpg)
![In cases where periapical drainage cannot be
established, Surgical Trephination is done.
Definition:
Trephination is the surgical perforation of alveolar
cortical plate [over the root end] to release the
accumulated tissue exudate that is causing pain.
[A small vertical incision is made adjacent to the tooth,
the mucosa is retracted and No.6 round bur is used to
penetrate cortical plate. This provides a drainage.]
Recent technique involves use of engine driven perforator
to enter the medullary bone with out the need of incision.
48](https://image.slidesharecdn.com/endodonticemergenciesfinal-151010115341-lva1-app6892/85/Endodontic-emergencies-48-320.jpg)
![Suggested Media:
Vestibule of mouth, Physiologic saline, Milk
Cell culture media, Hank's Balanced Salt Solution
[HBSS]
Milk
is considered the best medium because it has pH
& osmolality compatible to vital cells and
relatively free of bacteria and is readily available.
It maintains vitality of periodontal tissues for 3 hours.
Water
tooth should not be kept in water since it is a
hypotonic environment and leads to rapid cell lysis.
81](https://image.slidesharecdn.com/endodonticemergenciesfinal-151010115341-lva1-app6892/85/Endodontic-emergencies-81-320.jpg)