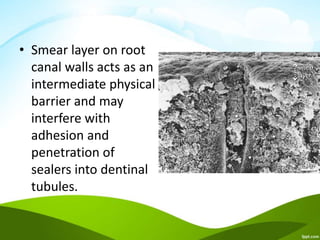
The document discusses the smear layer in endodontics, detailing its composition, significance, and the factors influencing its formation. It outlines the historical context of the smear layer's discovery, its effects on root canal treatment, and methods for its removal, emphasizing both its advantages and disadvantages in dental procedures. The presence of the smear layer can affect the sealing ability and bonding of dental materials, which impacts the outcome of endodontic treatments.