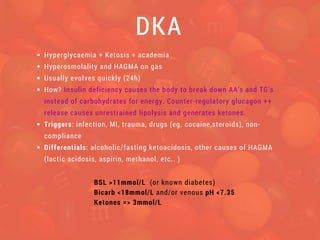
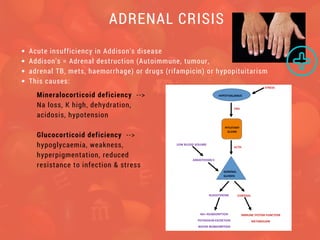
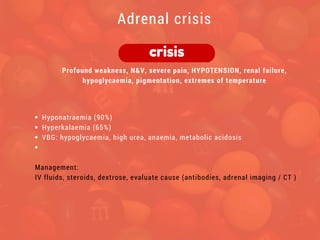
The most common endocrine emergencies are diabetic emergencies such as diabetic ketoacidosis (DKA) and hypoglycemia. Other less common but life-threatening emergencies include adrenal crisis, thyroid storm, hypoparathyroidism-related hypocalcemia, and pheochromocytoma. It is important to consider the diagnosis, triggers, and follow treatment protocols to stabilize the patient and address the underlying condition.