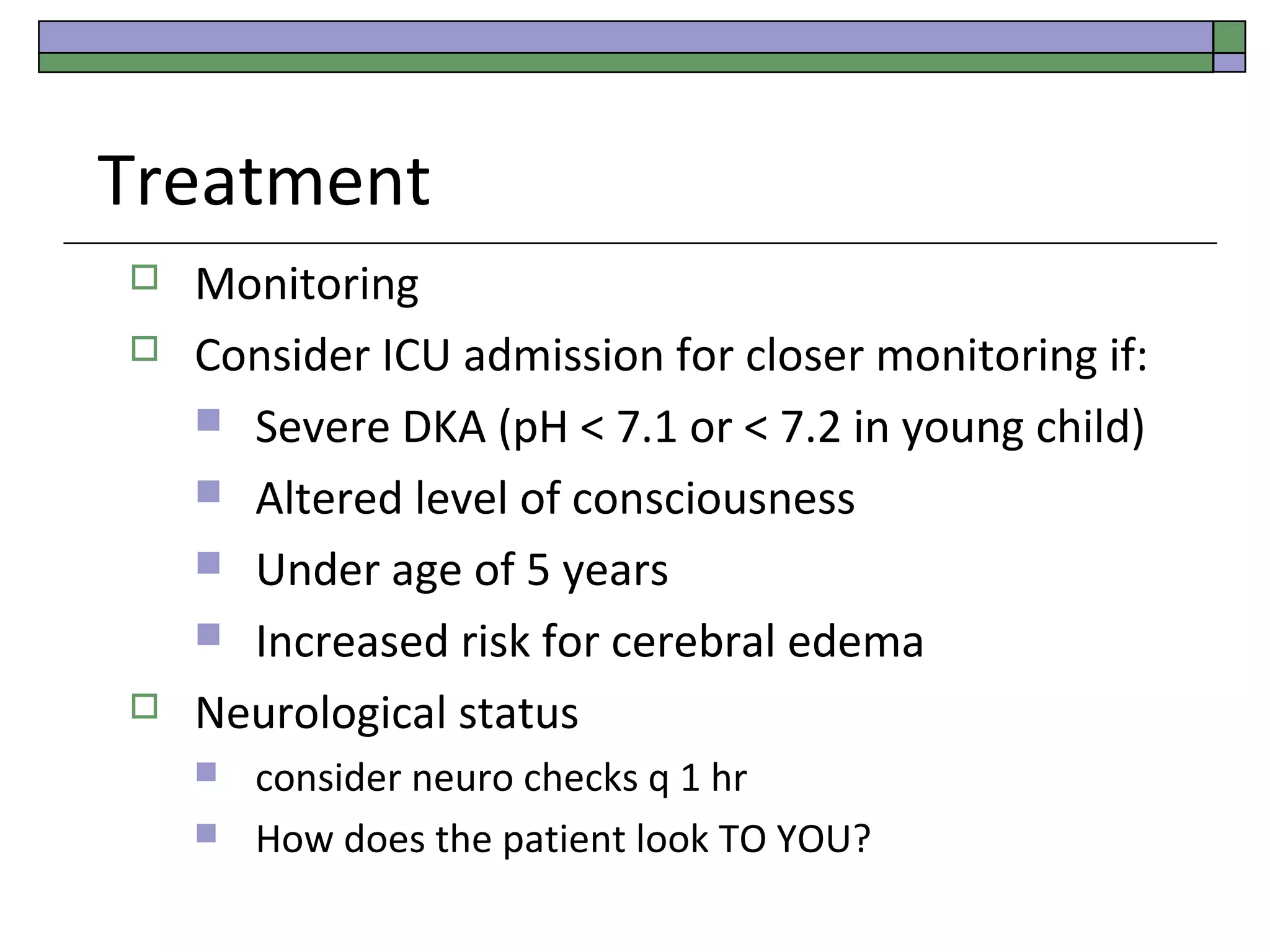
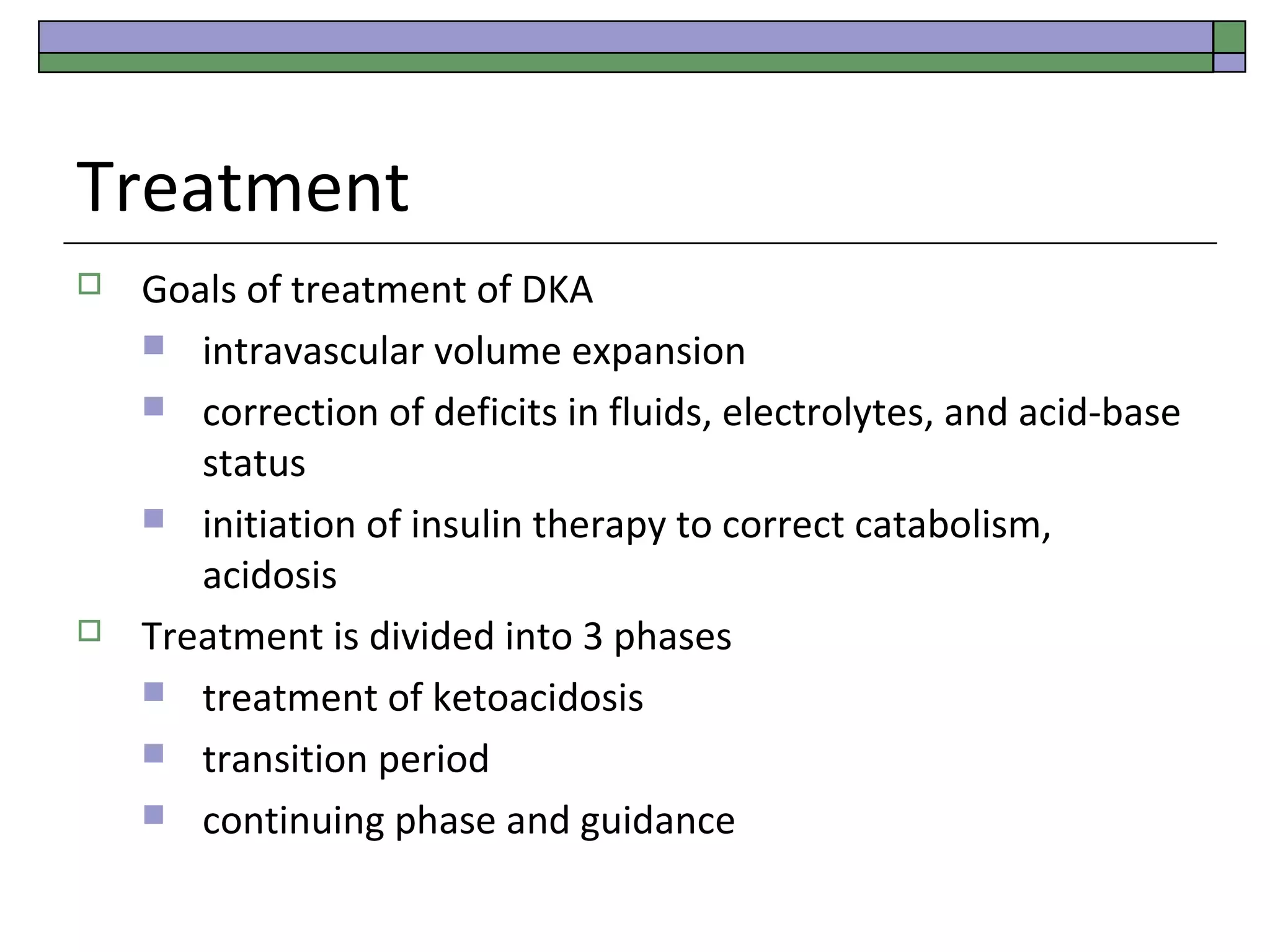
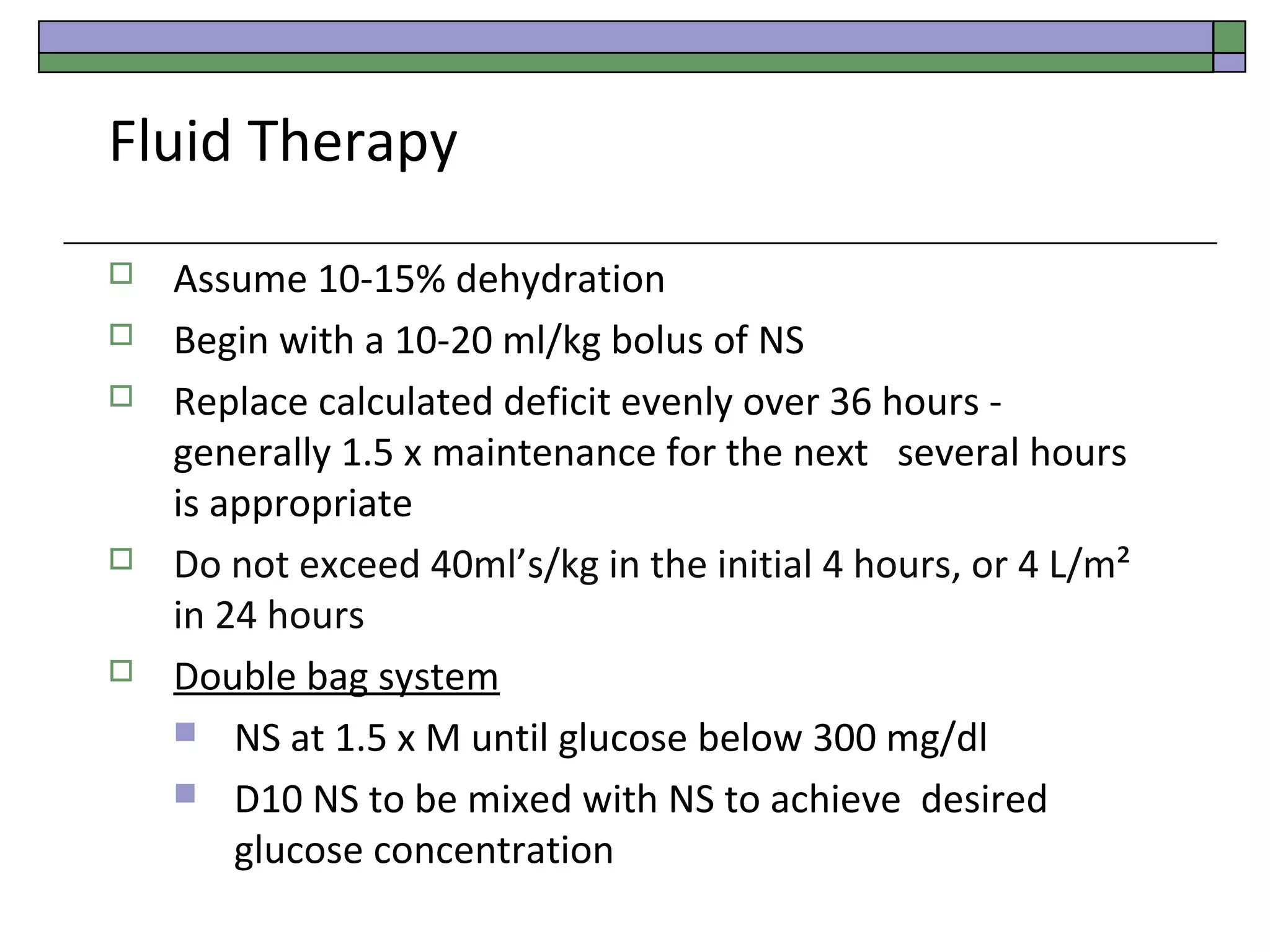
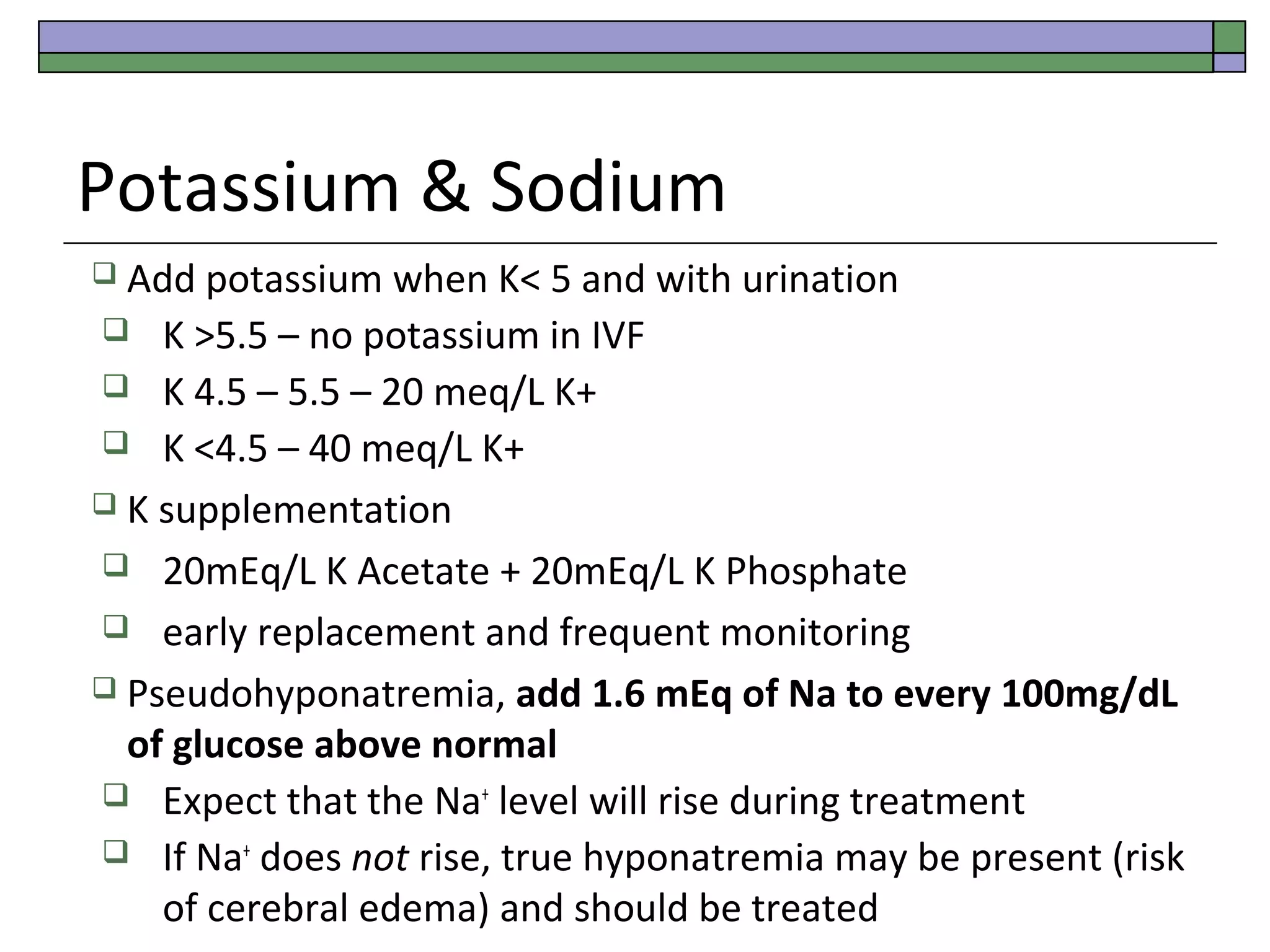
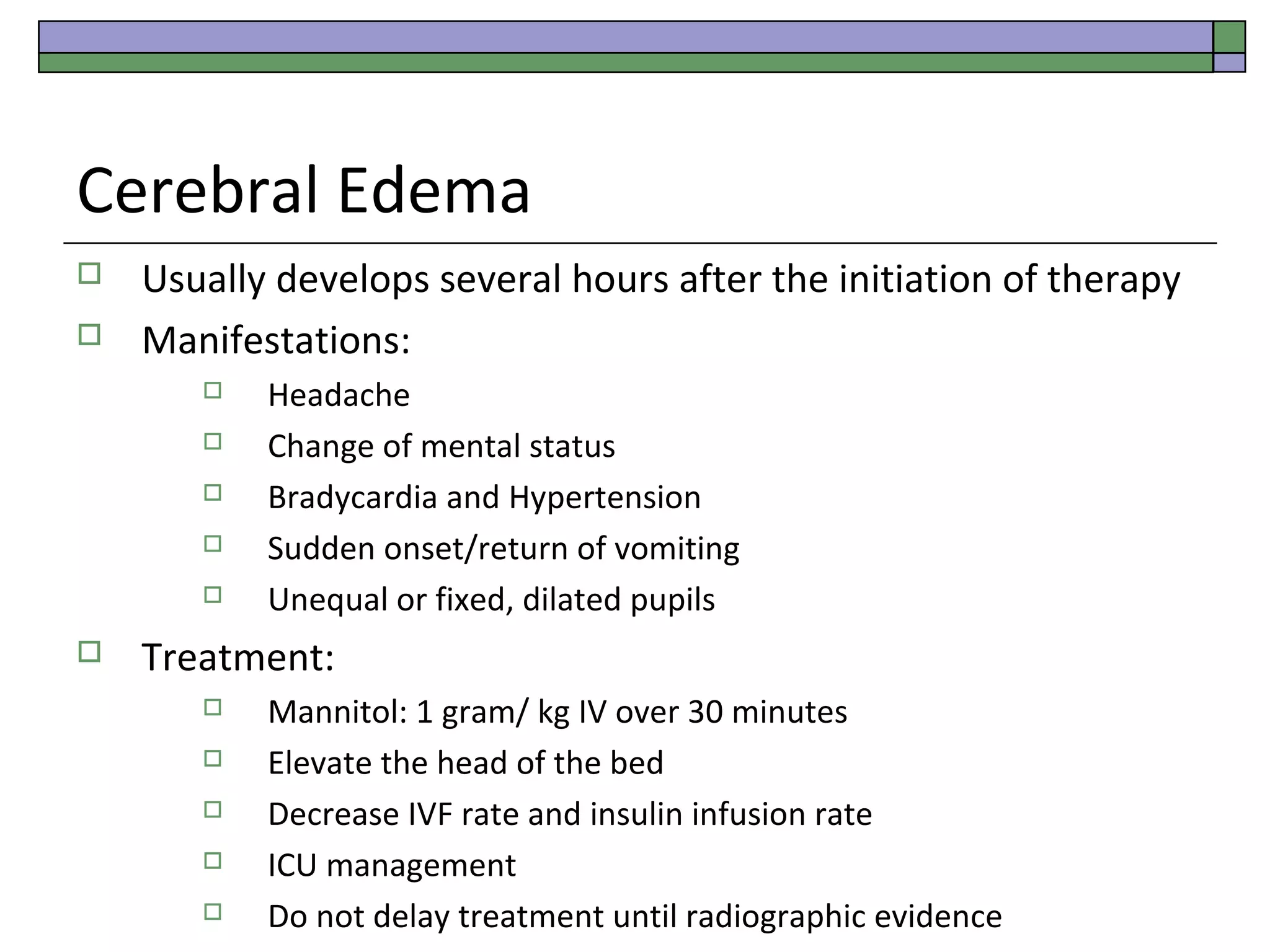
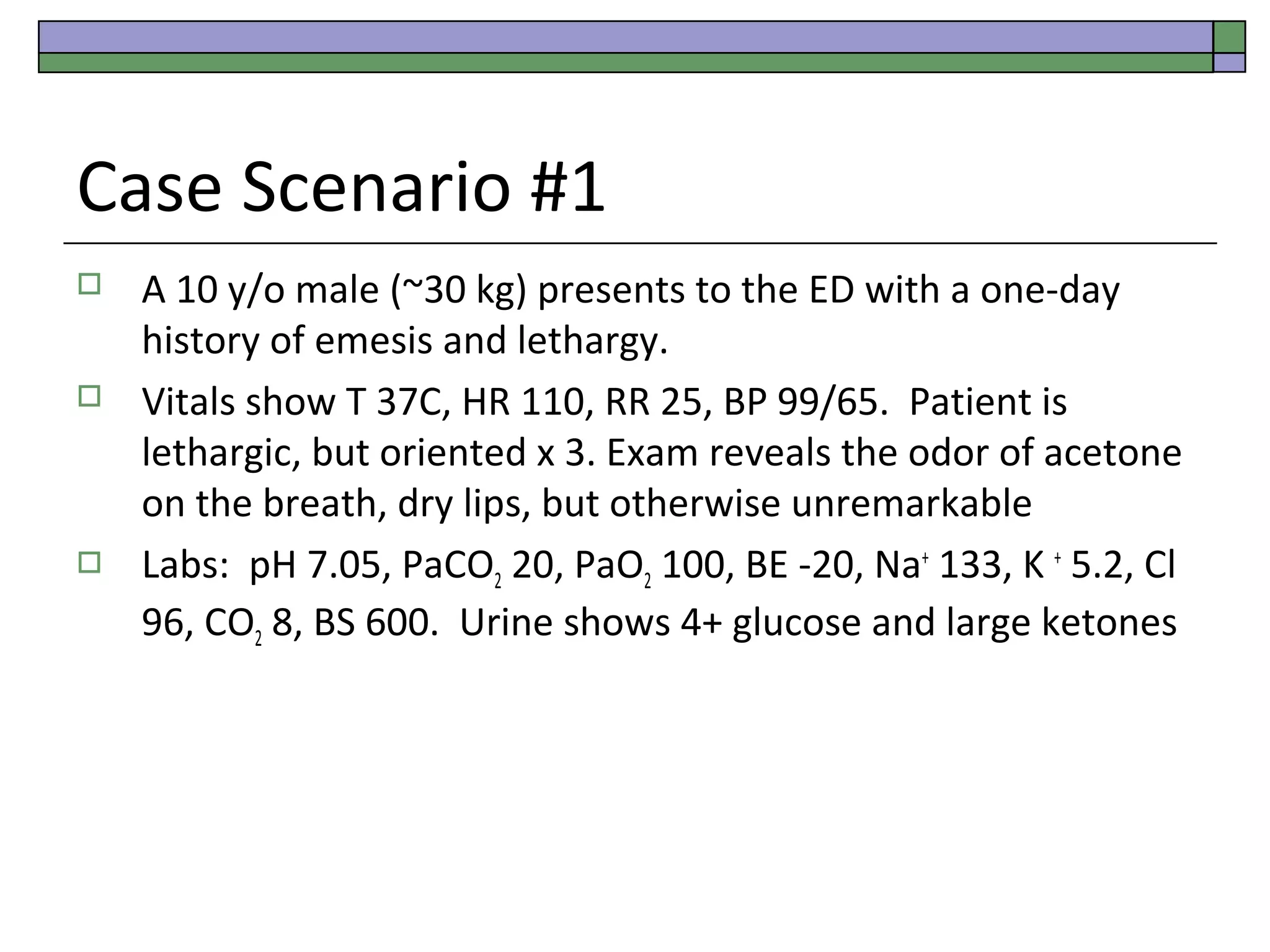
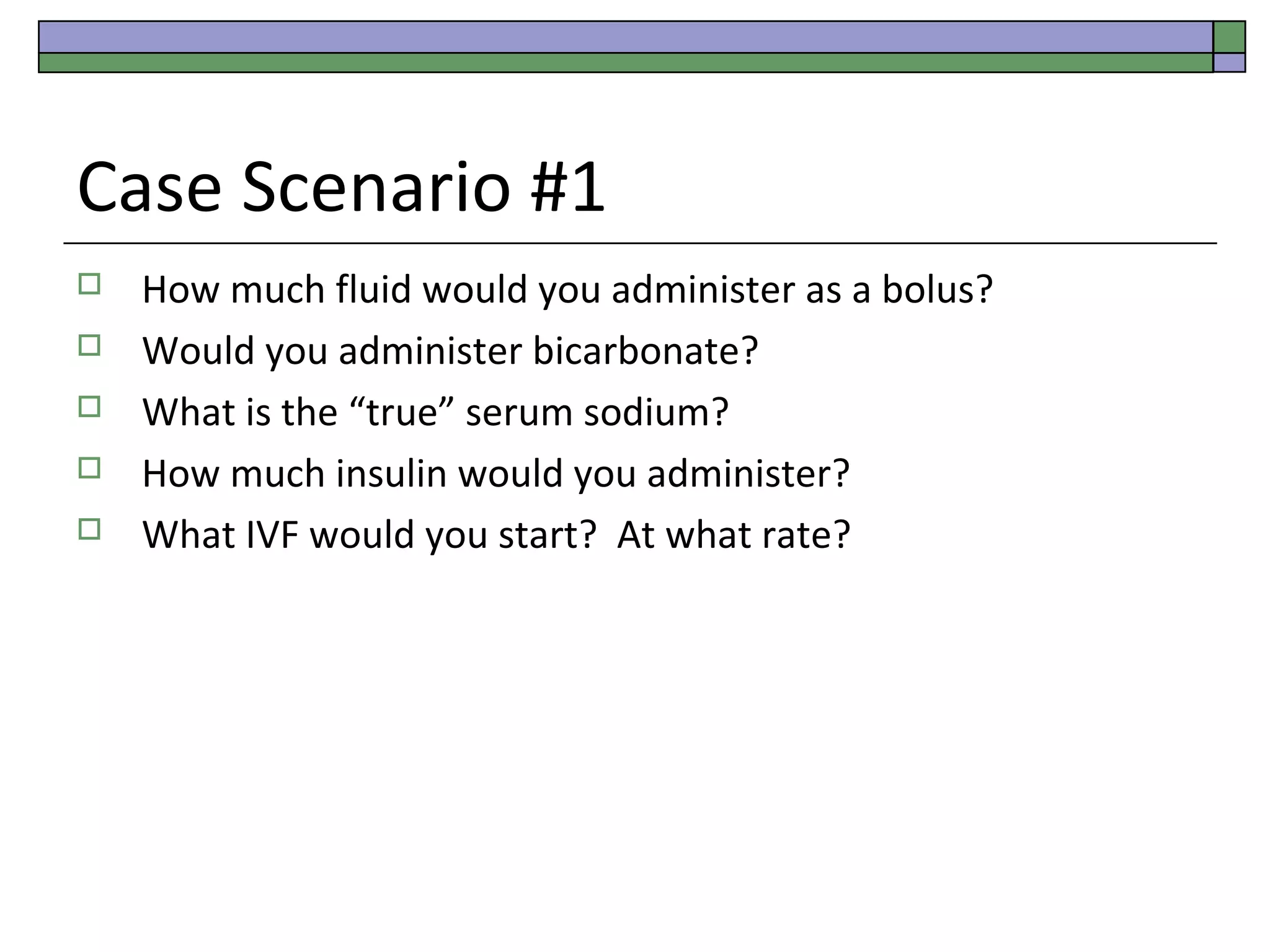
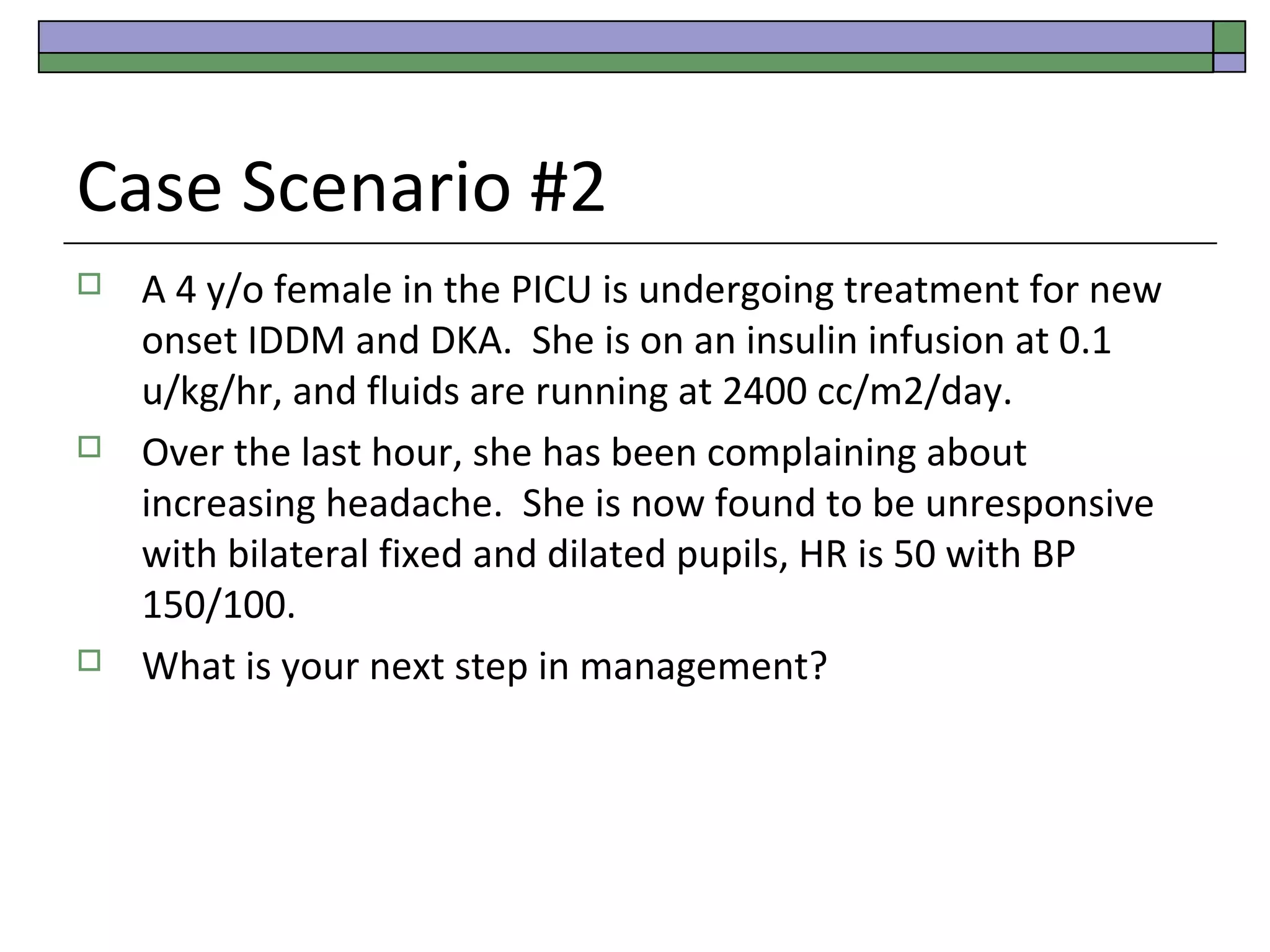
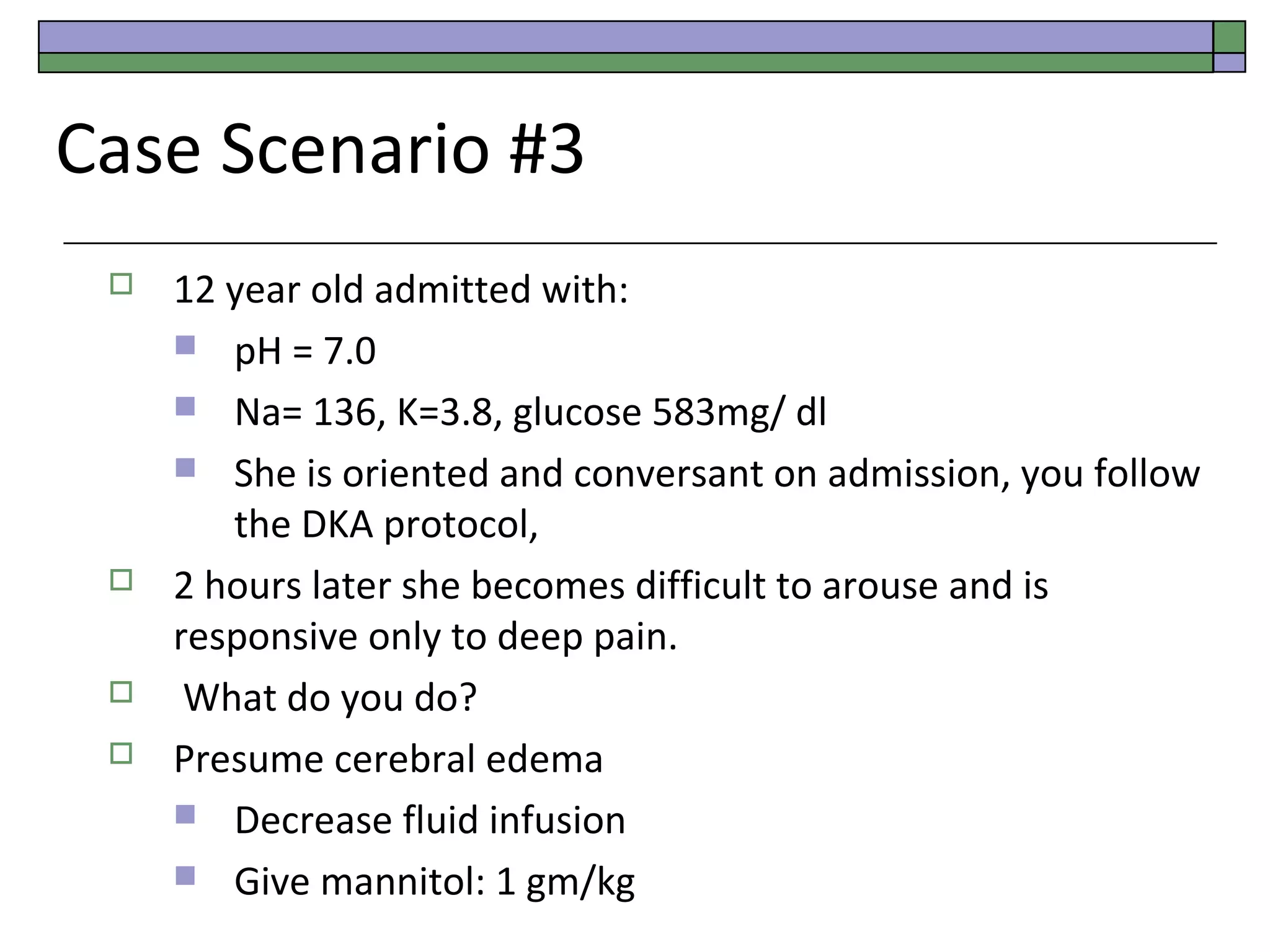
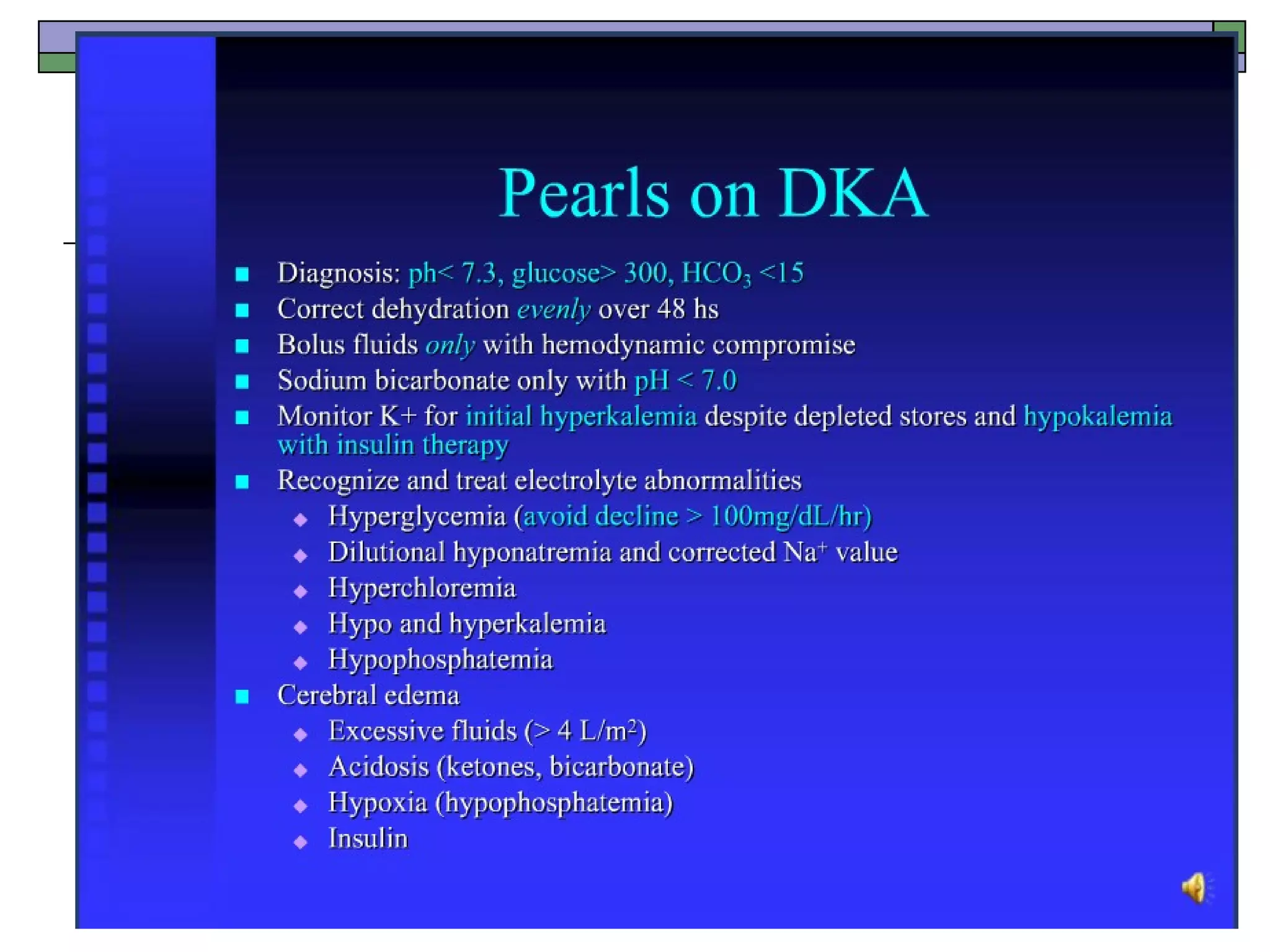
This document provides an overview of diabetic ketoacidosis (DKA), including its pathophysiology, diagnosis, treatment, and potential complications. It describes DKA as a serious complication of diabetes mellitus resulting from insulin deficiency and elevated counterregulatory hormones. The goals of treatment are fluid resuscitation, electrolyte replacement, and insulin therapy to reverse metabolic derangements while avoiding cerebral edema. Rapid treatment is important to reduce mortality, which can be up to 10% without treatment.