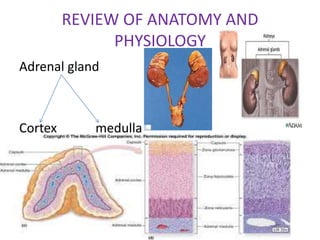
The document discusses several adrenal gland disorders including:
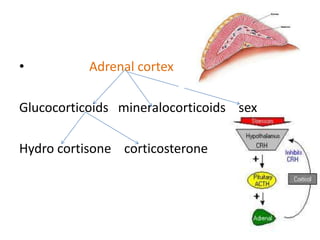
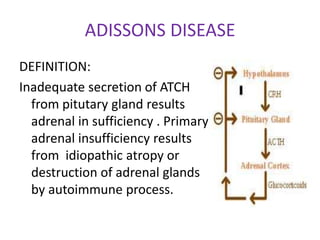
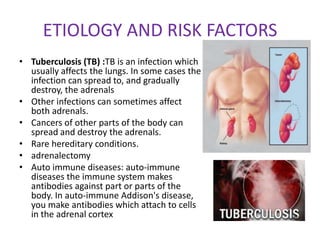
1. Addison's disease, which is caused by inadequate production of hormones by the adrenal glands due to problems with the pituitary gland or autoimmune destruction of the adrenal glands.
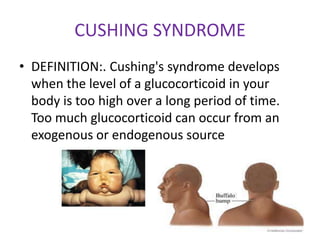
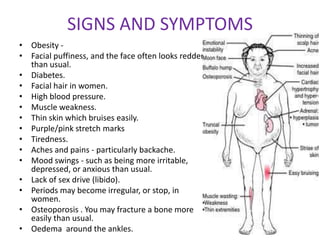
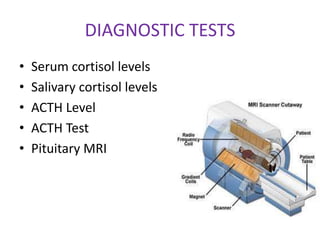
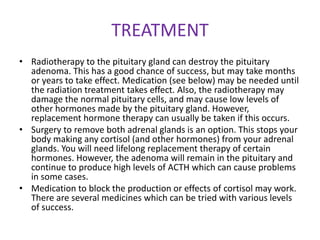
2. Cushing's syndrome, which is caused by excessive cortisol production from either benign or cancerous tumors of the adrenal glands or pituitary gland.
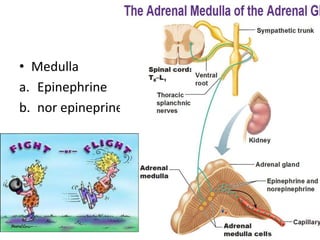
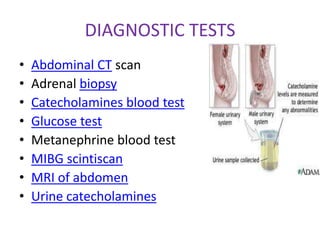
3. Pheochromocytoma, a rare tumor of the adrenal medulla that secretes excess catecholamines and causes symptoms like headaches and sweating.
4. Testing of the corticotropin-releasing factor is discussed as a way to diagnose hypothal