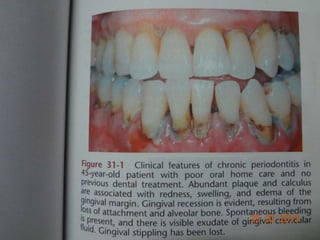
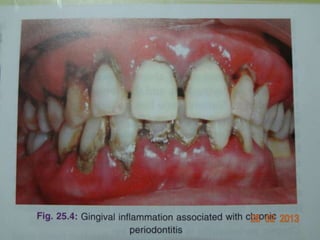
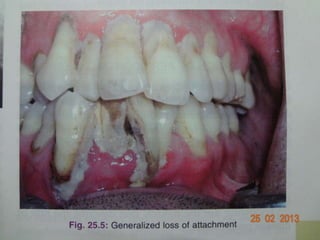
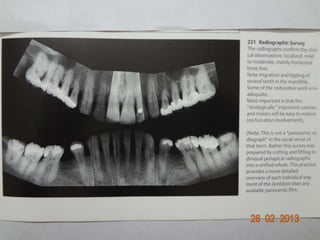
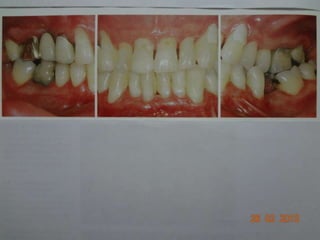
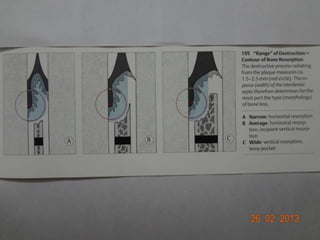
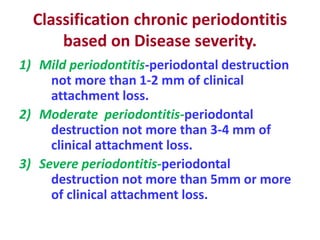
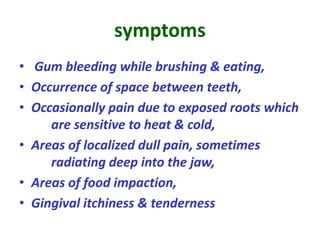
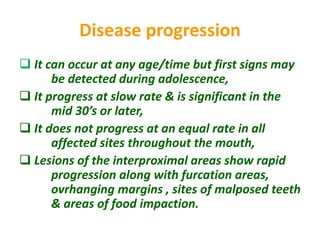
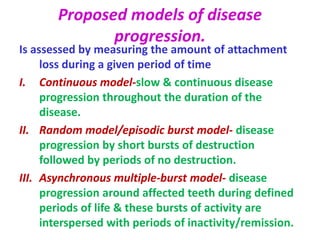
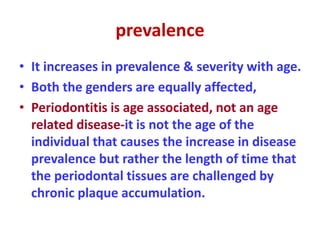
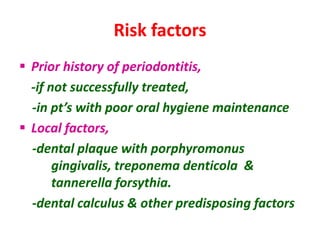
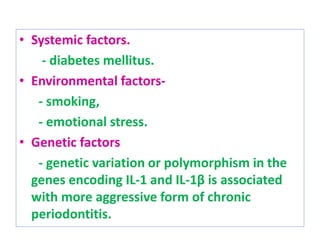
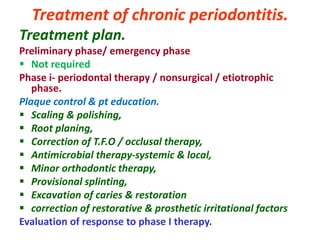
Chronic periodontitis is an infectious disease that results in inflammation of the gums and bones supporting the teeth. It is characterized by progressive gum attachment loss and bone loss over time. Symptoms include bleeding gums, spaces opening between teeth, and occasional pain. Risk factors include poor oral hygiene, smoking, diabetes, and genetic factors. Treatment involves nonsurgical approaches like deep cleaning below the gumline to remove bacterial plaque and tartar, followed by surgical procedures if needed. Regular maintenance care is important to prevent further progression of the disease.