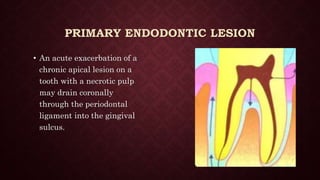
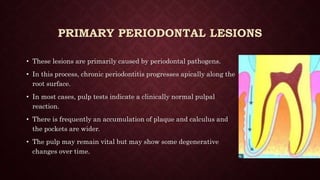
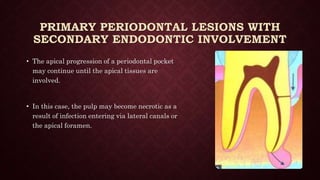
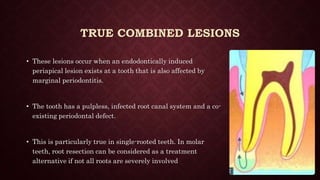
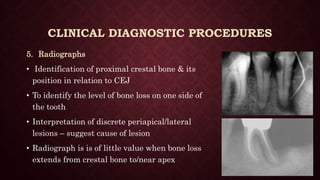
This document discusses endo-perio lesions, which involve both endodontic and periodontal tissues. It defines endo-perio lesions as involving pulpal disease and destruction of the attachment apparatus from the gingival sulcus to the apex. There are anatomical and non-anatomical pathways connecting the tissues. Lesions are classified based on whether the primary involvement is endodontic or periodontal. Diagnostic procedures and appropriate treatment depend on accurately distinguishing the primary pathology. Treatment may involve endodontic therapy, periodontal therapy, or both depending on the classification and extent of disease.