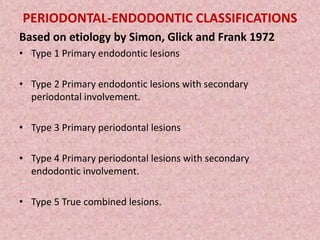
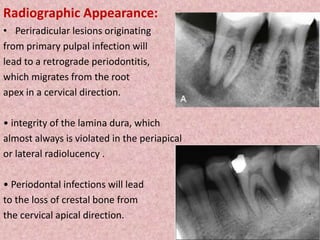
The periodontic-endodontic continuum describes how pulpal and periodontal diseases are interrelated and can influence each other. Pulpal infections can spread retrograde through the apical foramen and cause periodontal bone loss, while advanced periodontitis can spread infection into the pulp through lateral canals or dentinal tubules. It is important to differentiate between primary endodontic or periodontal lesions, and lesions that involve both tissues. Treatment may require endodontic therapy, periodontal therapy, or both depending on the diagnosis. Procedural accidents during endodontic treatment like perforations or sodium hypochlorite accidents can also impact the periodontium.