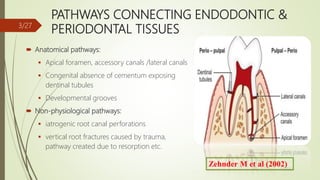
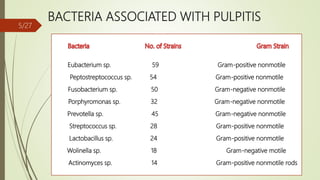
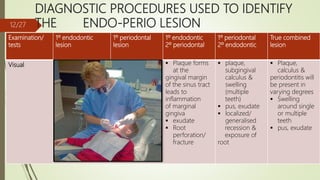
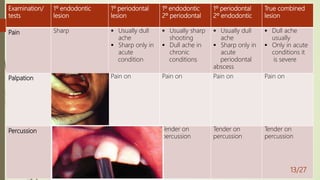
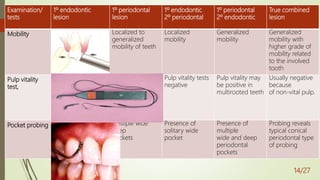
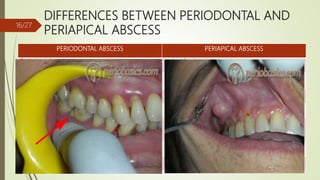
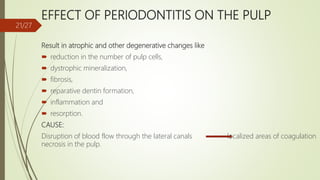
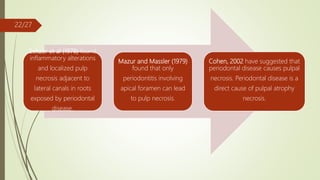
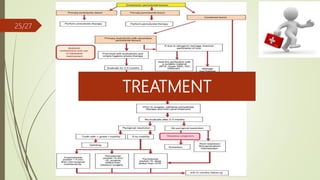
This document provides an overview of endodontic-periodontal interactions. It discusses the pathways connecting endodontic and periodontal tissues, the etiology of endo-perio lesions, classifications of endo-perio lesions, diagnostic procedures, differences between periodontal and periapical abscesses, the endo-perio controversy, and management of pulpal and periodontal diseases. The key relationships covered are the anatomical and pathological connections between the pulp and periodontium, the bacteria commonly found in both tissues, and the debate around whether periodontal or endodontic disease can cause the other.