This document discusses periodontal-endodontic lesions, including:
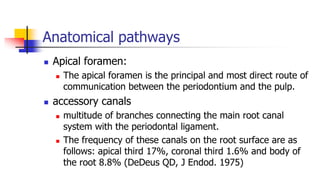
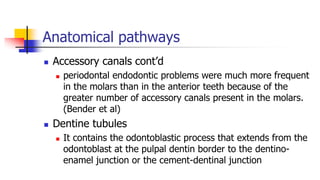
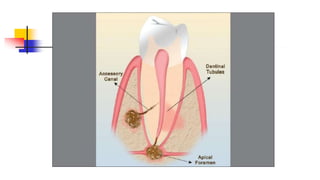
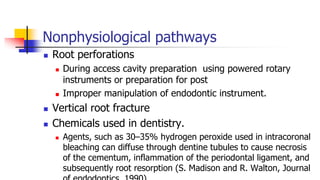
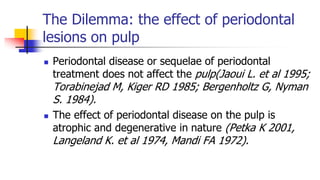
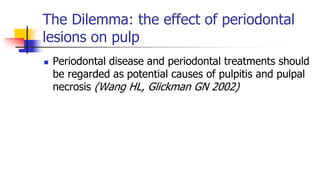
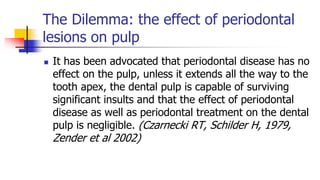
- The relationship between the periodontium and pulp and pathways of communication between them.
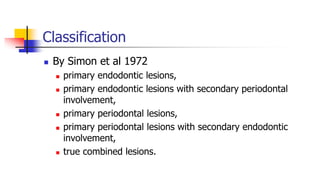
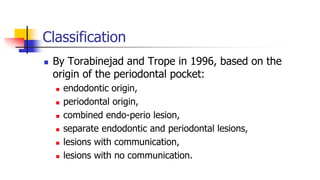
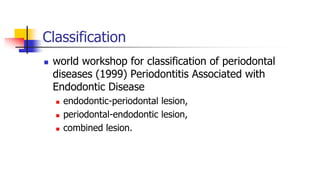
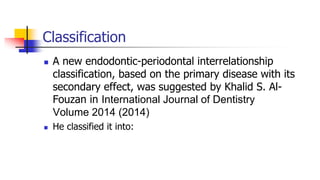
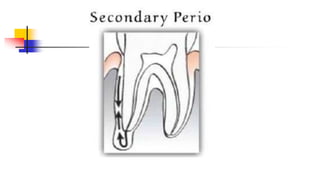
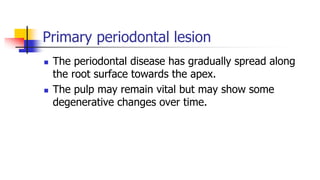
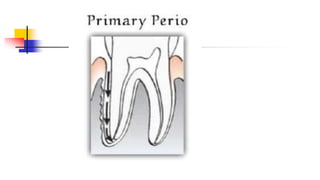
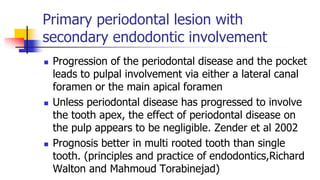
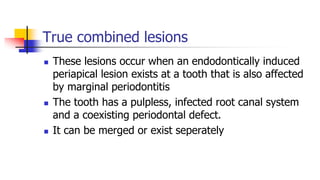
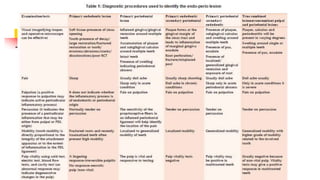
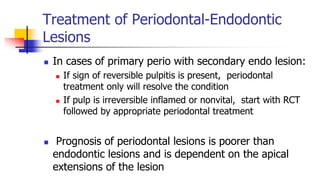
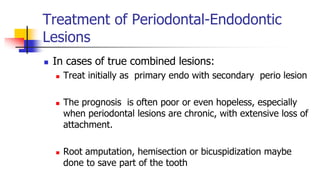
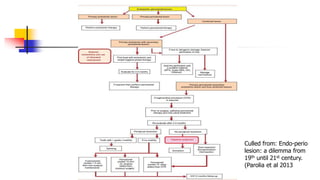
- Classifications of lesions based on origin as primary endodontic, periodontal, or combined.
- Diagnosis involves determining the origin of the lesion and ruling out other causes.
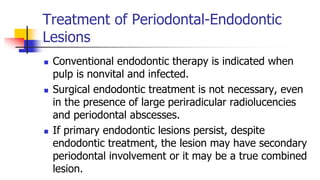
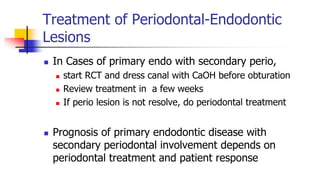
- Treatment depends on the classification but generally involves endodontic treatment, periodontal treatment, or both to fully resolve the lesion. Prognosis depends on the extent and chronicity of the periodontal involvement.