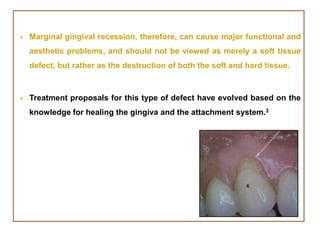
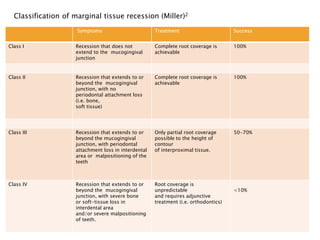
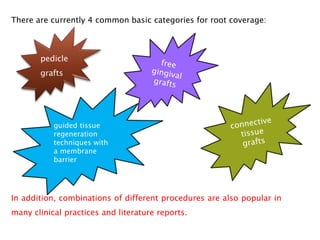
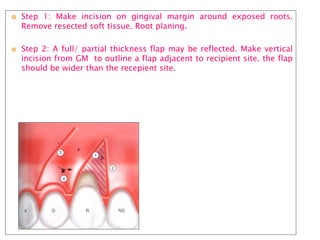
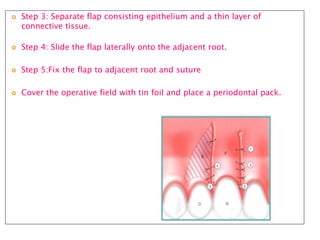
Gingival recession is the displacement of gingival tissue away from the tooth surface, exposing the root surface. It can be caused by periodontal disease, traumatic brushing, occlusal issues, or iatrogenic factors. Treatment depends on the severity and classification of the recession. For mild cases with no sensitivity or aesthetic concerns, improved brushing may suffice. More severe recession involving sensitivity or aesthetics may be treated with surgical root coverage procedures like laterally positioned pedicle grafts or coronally advanced flaps, which can achieve 65-98% root coverage depending on the technique and recession classification. The laterally positioned pedicle graft involves sliding keratinized gingiva from an adjacent tooth to cover the exposed root