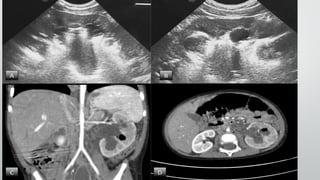
This document discusses emphysematous pyelonephritis (EPN), a severe necrotizing renal infection characterized by gas formation in the renal parenchyma and tissues. It presents 4 case studies of EPN and provides details on etiology, risk factors, diagnosis and treatment. EPN most commonly affects women and diabetics. Imaging such as ultrasound and CT scan can diagnose the condition by detecting gas in the kidneys and tissues. Treatment involves antibiotics, drainage of pus and fluids, and sometimes nephrectomy, with the current approach being percutaneous drainage and antibiotics to try to save the kidney.