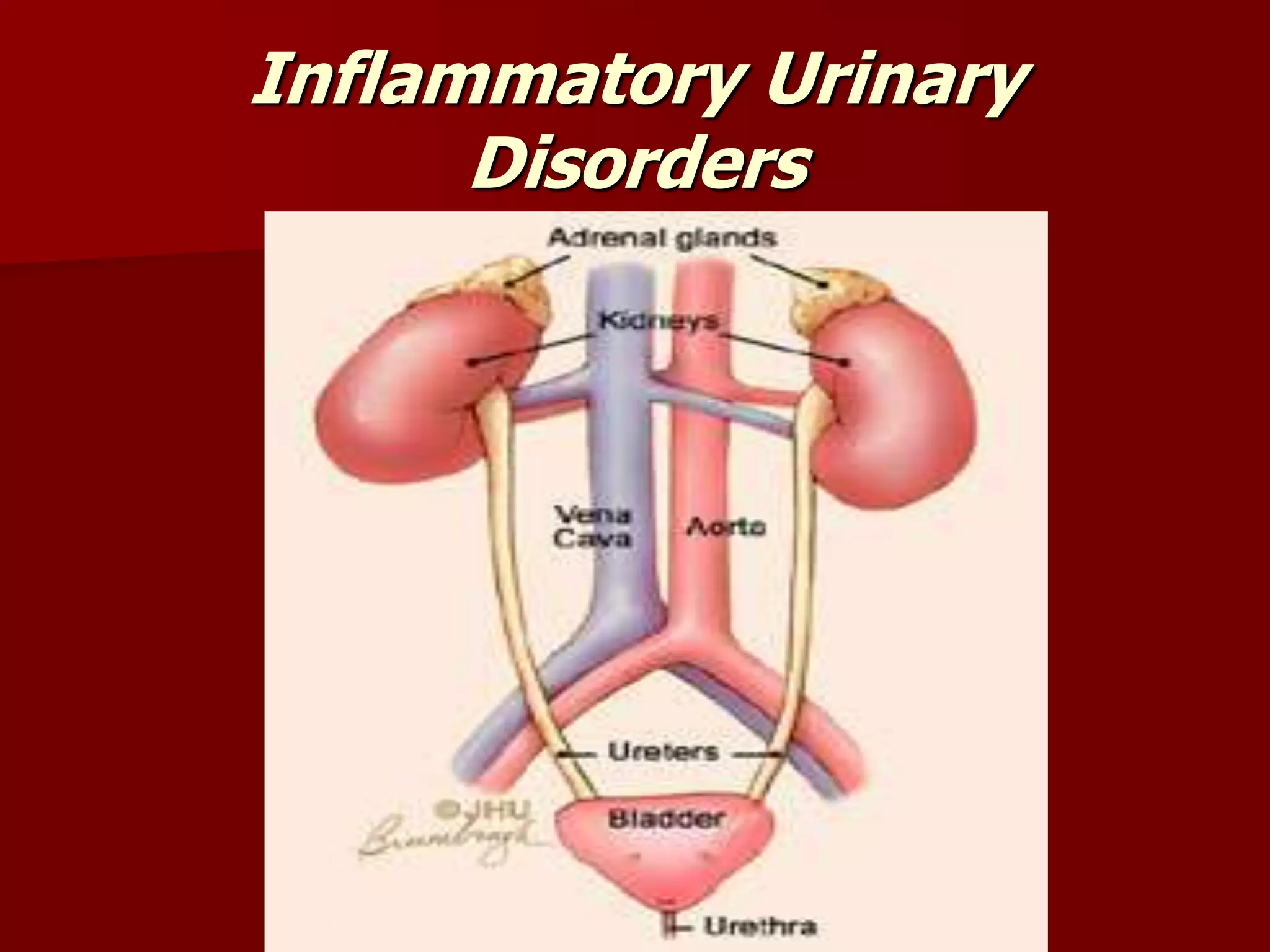
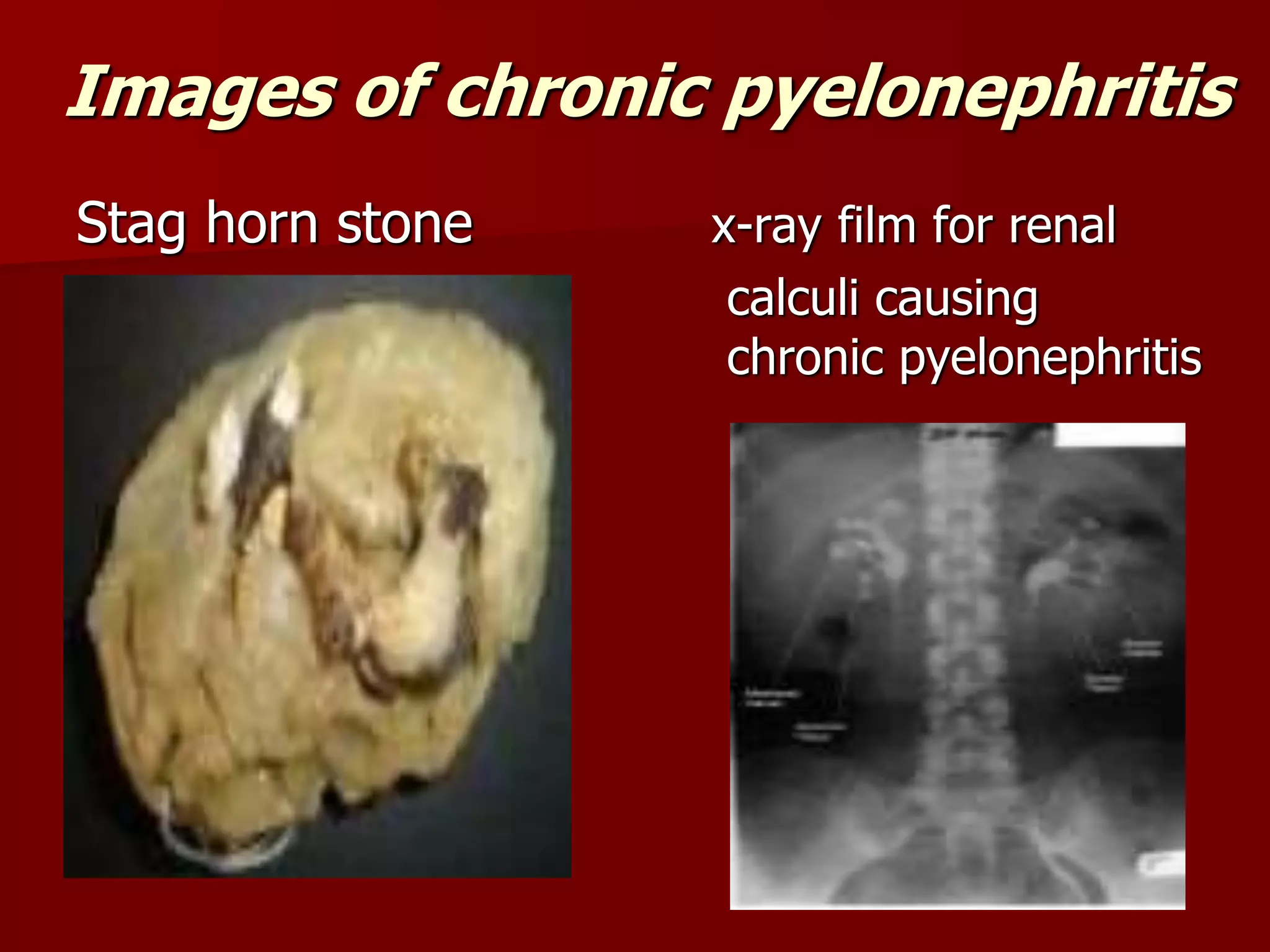
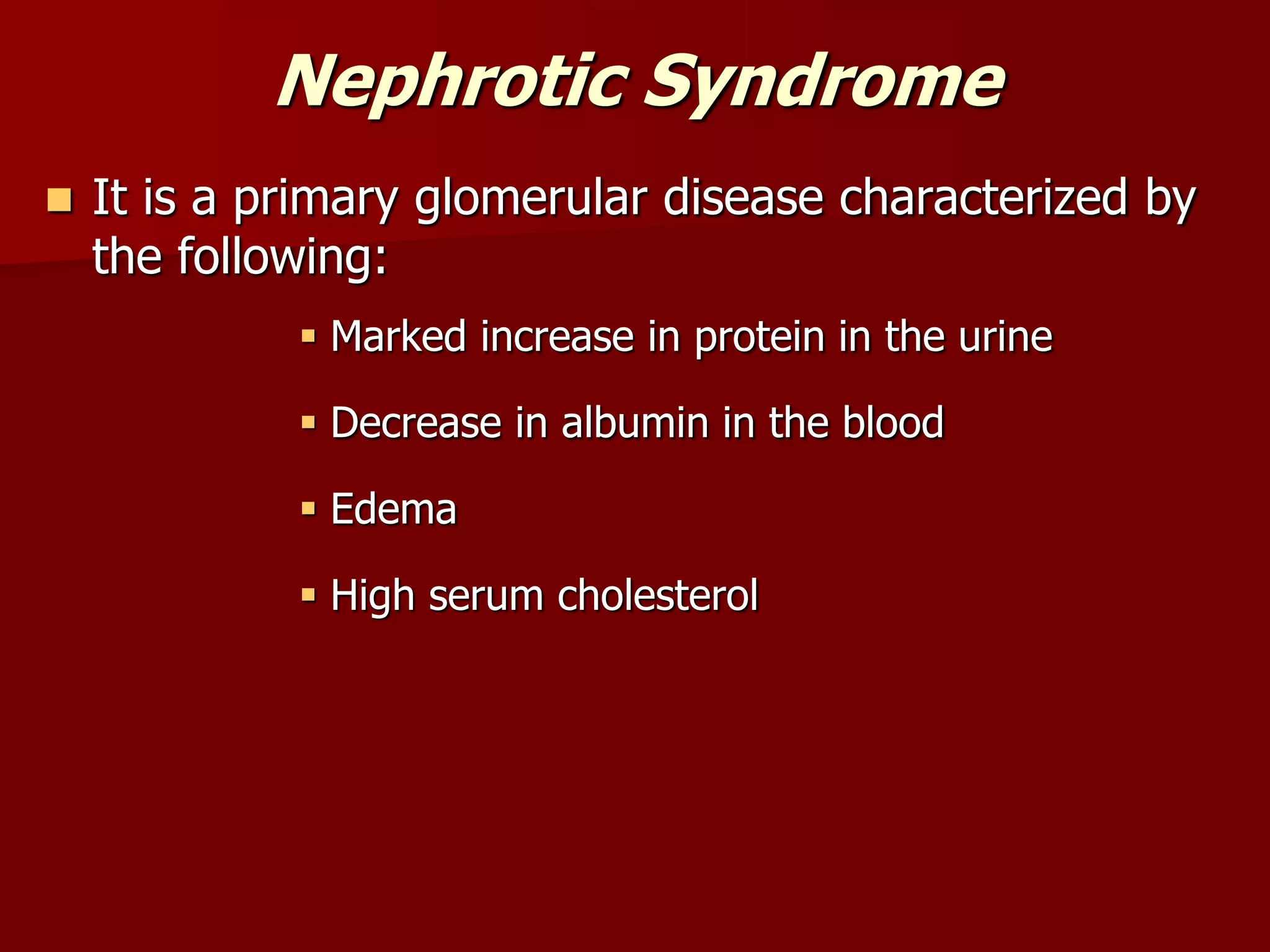
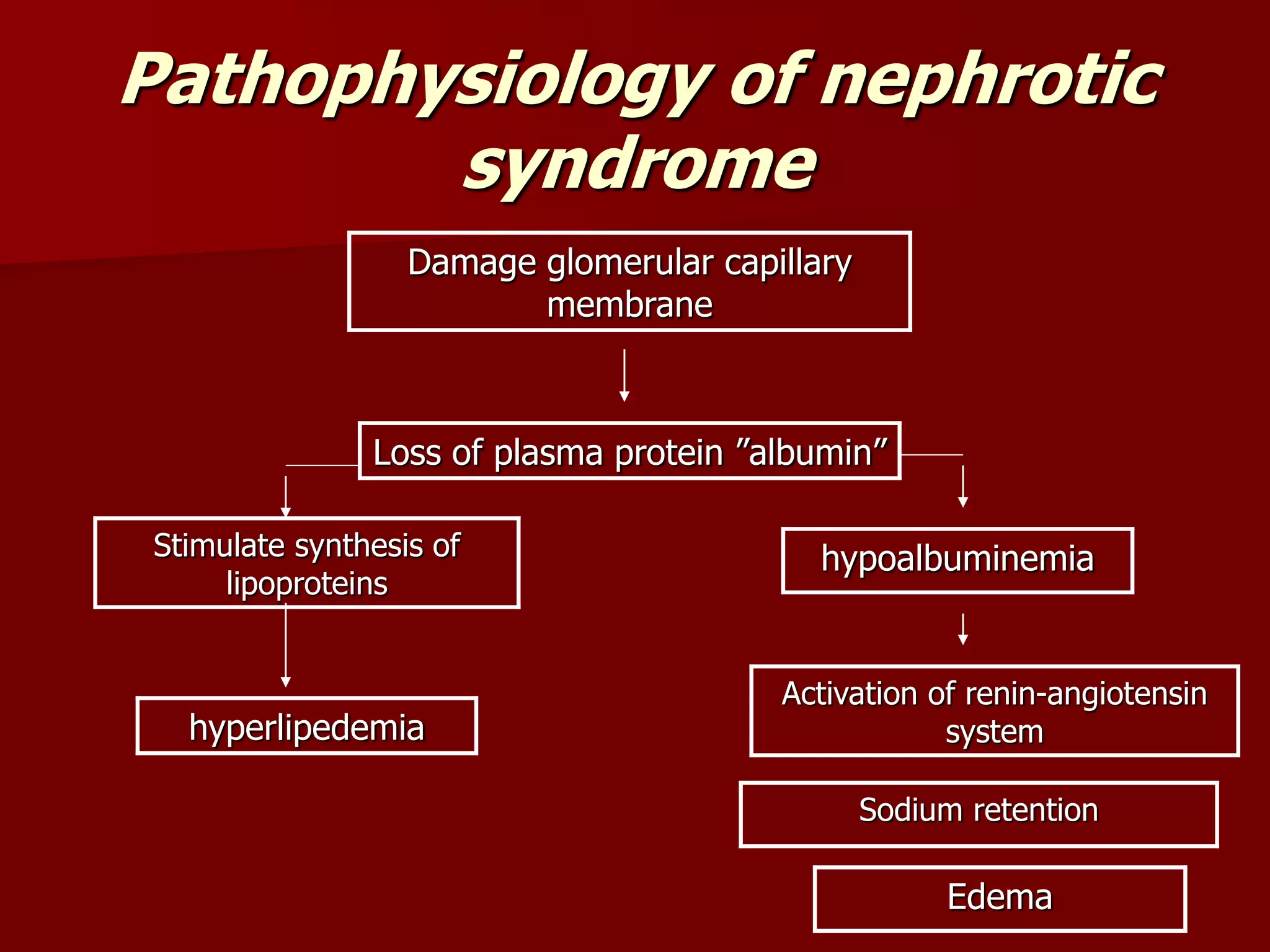
This document discusses various inflammatory urinary disorders including urinary tract infections, pyelonephritis, chronic cystitis, glomerular diseases, and nephrotic syndrome. It covers the pathophysiology, risk factors, clinical manifestations, diagnostic findings, medical management, and nursing care for each condition. Urinary tract infections can be upper or lower and are common in women. Pyelonephritis is a kidney infection that may be acute or chronic. Chronic cystitis involves long-term inflammation and scarring of the bladder wall. Glomerular diseases damage the kidney filters and include acute and chronic glomerulonephritis. Nephrotic syndrome is a kidney disorder defined by protein in the urine and low