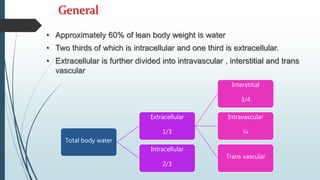
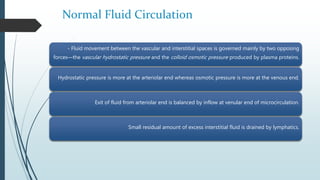
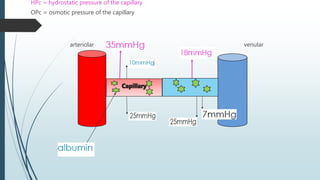
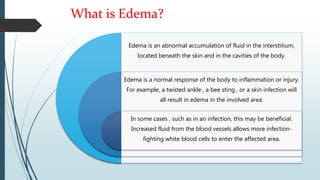
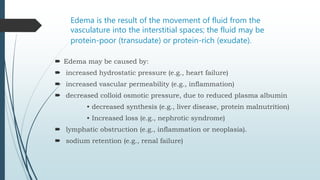
Edema is an abnormal accumulation of fluid in the interstitium caused by an imbalance of hydrostatic and oncotic pressures that pushes fluid into tissues. It can be caused by increased hydrostatic pressure, increased vascular permeability, or decreased plasma oncotic pressure due to low albumin. Treatment focuses on resolving the underlying cause and improving drainage of fluid from tissues.