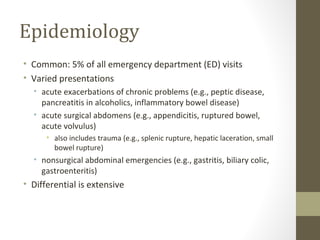
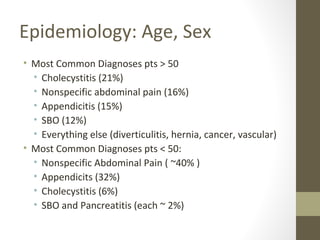
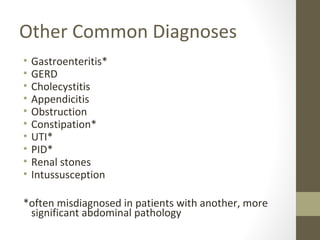
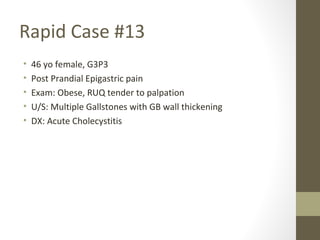
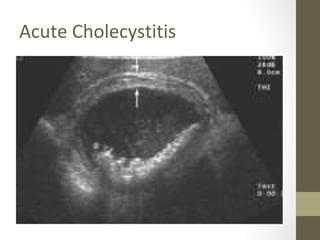
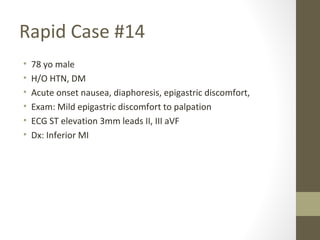
The lecture covers the evaluation and management of abdominal pain in emergency department patients, highlighting common causes, the importance of thorough history and physical examination, and the necessity for timely intervention. It details demographics, presenting symptoms, and an extensive differential diagnosis, emphasizing life-threatening conditions that could arise in various age groups. Key considerations such as pain assessment, diagnostic tests, and management approaches are also discussed to guide medical decision-making.