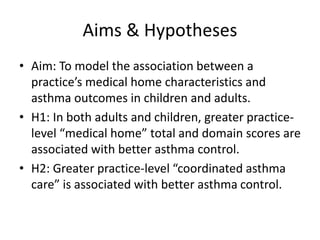
This document describes the design and methods of a prospective cohort study examining the association between practice-level medical home characteristics and asthma outcomes in children and adults. The study will use surveys of medical home characteristics and secondary data from 2011-2013. Asthma control and exacerbations will be measured repeatedly from July 2012 to December 2013. Hierarchical linear models will assess the relationship between medical home scores and asthma outcomes, adjusting for potential confounders. Sensitivity analyses will address issues like misclassification bias. Results will be presented separately for children and adults.