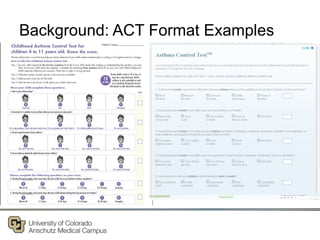
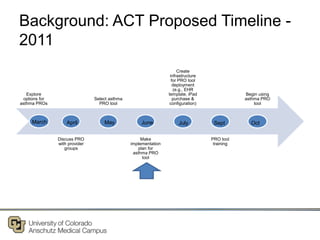
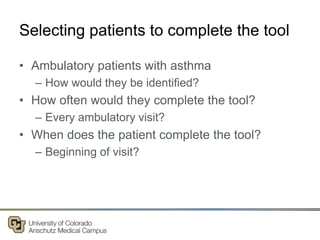
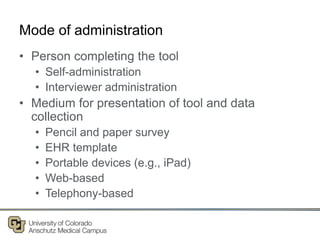
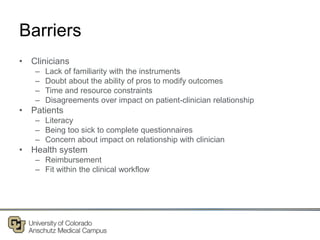
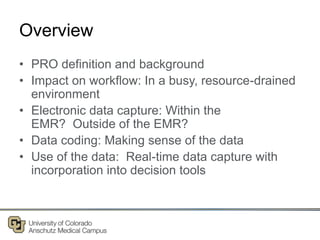
The document discusses implementing point-of-care patient-reported outcomes (PROs) in clinical settings, particularly focusing on the Asthma Control Test (ACT) as a tool for improving patient care. It outlines the necessity for data capture, workflow considerations, and the importance of patient-centered care alongside challenges such as clinician familiarity and patient literacy. The implementation plan includes resource allocation, patient identification, and evaluating the tool's effectiveness in practice.