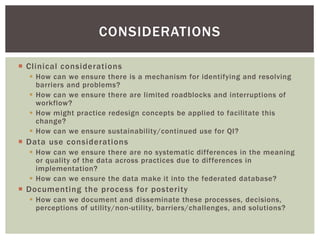
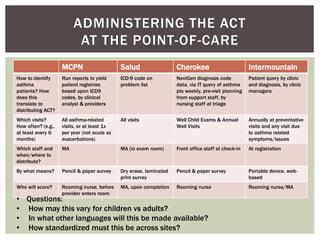
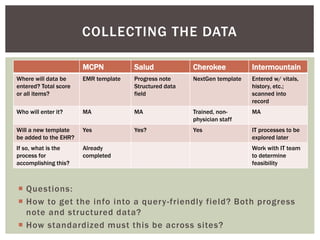
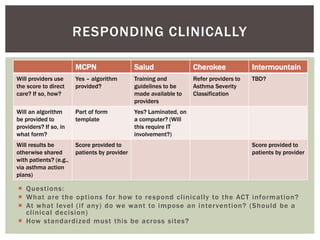
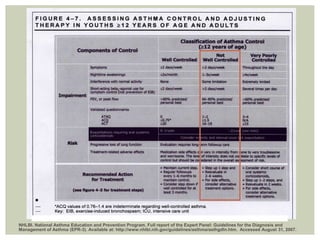
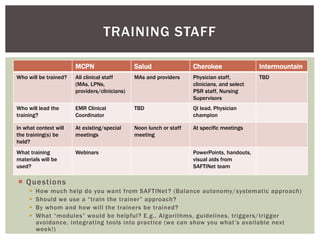
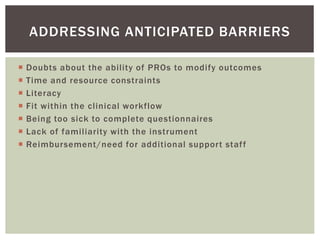
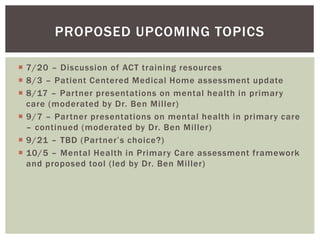
The document discusses the implementation of asthma care initiatives, focusing on identifying asthma patients, data collection methods, and clinical responses to the Act information. It raises questions regarding workflow barriers, data standardization, and the training of clinical staff. Additionally, it highlights anticipated challenges such as resource constraints and patient literacy while proposing future discussions and training resources.