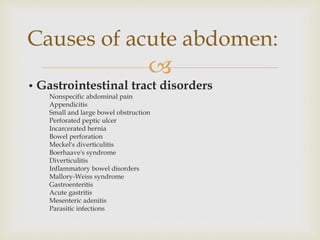
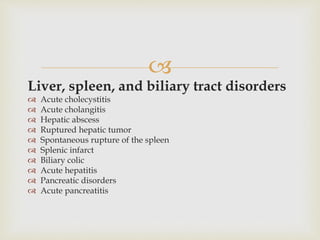
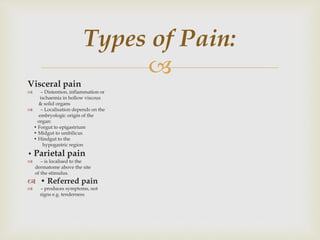
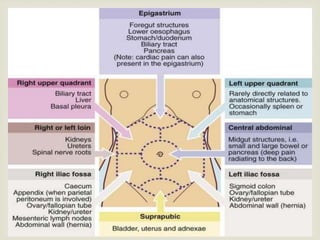
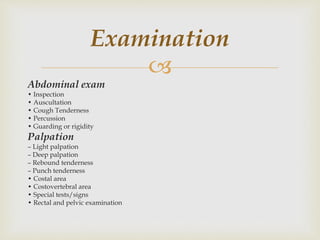
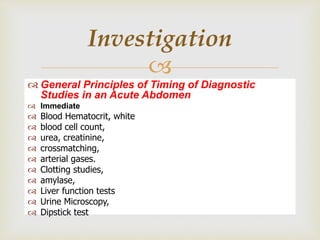
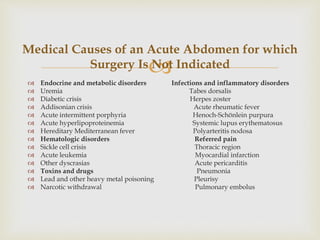
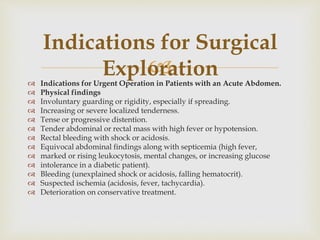
This document discusses the case of a patient named Abdul Rehman who was admitted to the hospital with acute abdominal pain after recently having his right leg amputated following an accident. The patient was initially resuscitated with IV fluids and other measures. Exploratory laparotomy was planned due to findings of free fluid in the abdomen. The document then provides information on defining an acute abdomen, common causes, characteristics of pain, examination techniques, investigations, initial resuscitation measures, pre-operative management, non-surgical causes, and indications for surgical exploration.