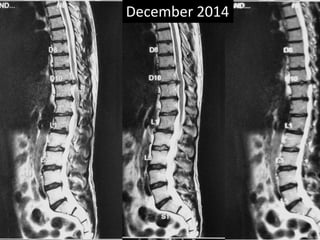
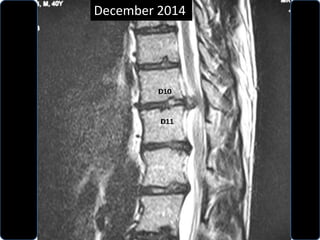
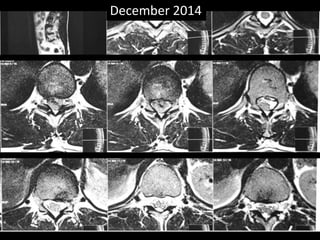
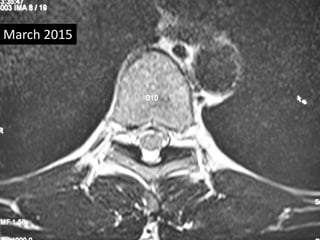
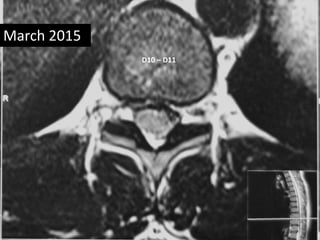
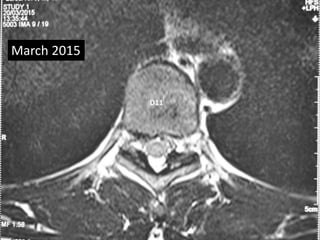
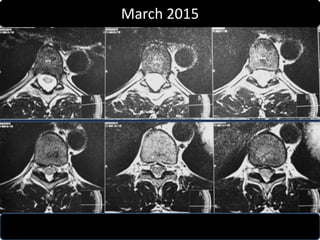
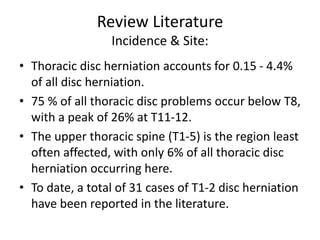
A 40-year-old male gymgoer experienced sudden weakness and parasthesia in his right lower limb while weight lifting. He regained control of his limb within 15 minutes with massage. MRI revealed a disc extrusion at D10-D11. He was treated conservatively with observation, precautions, and instructions to report any worsening symptoms. A follow up MRI showed complete absorption of the disc fragment. Thoracic disc herniations typically occur below T8 and account for under 5% of all disc herniations. They are usually treated conservatively but surgery may be required for myelopathy, progressive weakness, or intolerable pain.