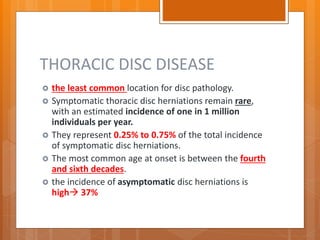
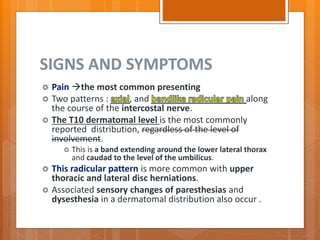
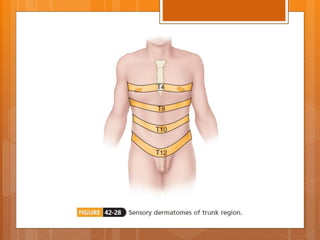
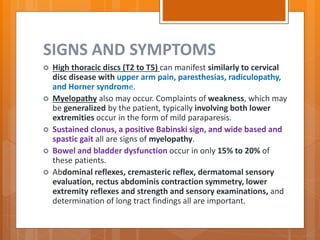
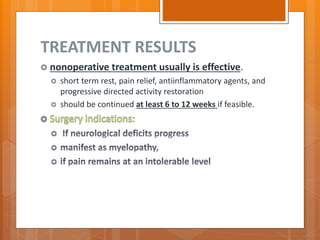
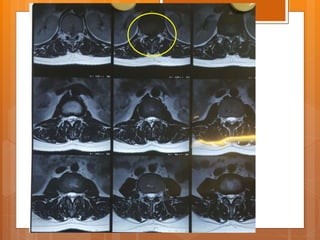
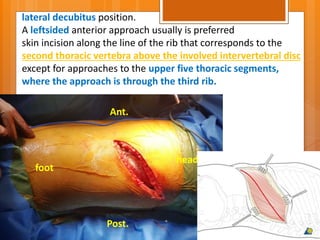
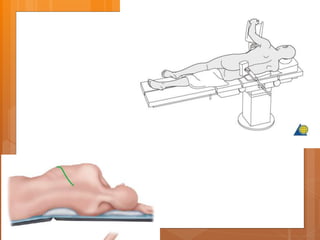
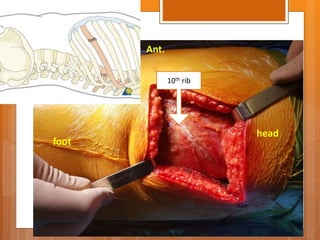
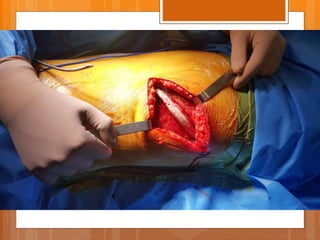
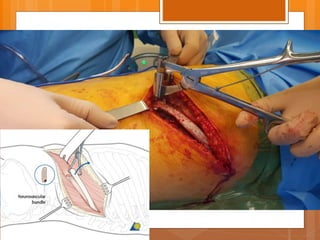
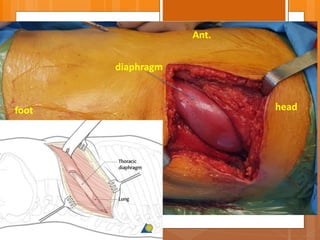
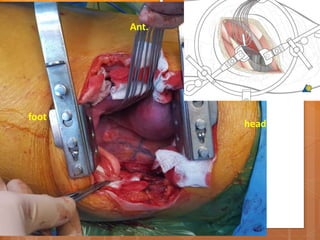
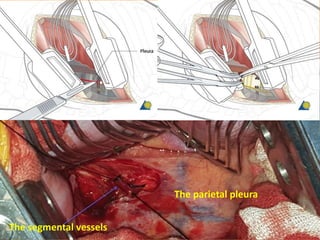
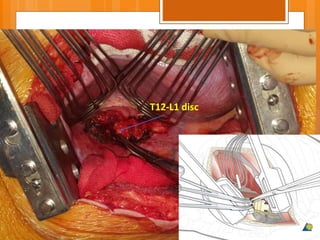
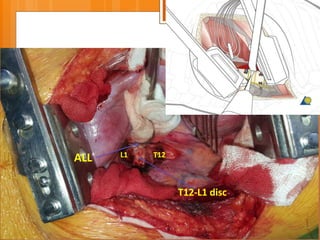
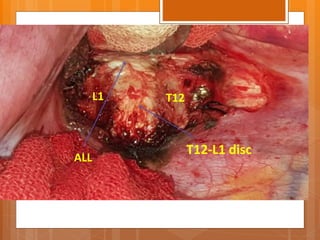
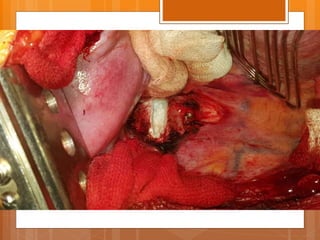
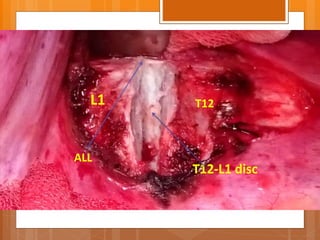
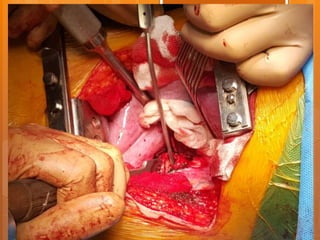
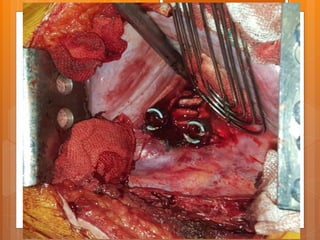
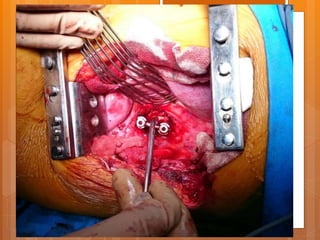
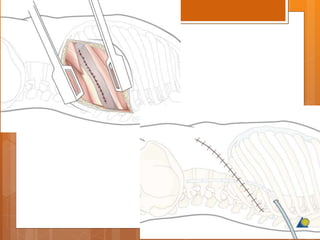
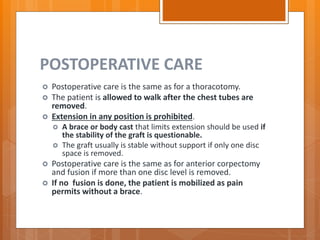
This document discusses thoracic disc disease, which affects the thoracic spine. Thoracic disc herniations are rare, representing 0.25-0.75% of all disc herniations. The most common symptoms are pain between the shoulder blades and along the intercostal nerves, with the T10 dermatome most commonly affected. Treatment typically begins with rest, anti-inflammatories, and physical therapy, with surgery such as anterior discectomy reserved for cases that do not improve with conservative care. Anterior surgical approaches involve entering through the chest wall between the ribs to access and remove herniated disc material compressing the spinal cord or nerves.