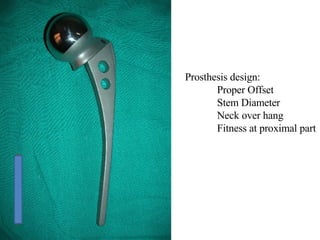
1) Proper proximal fixation of the femoral implant is crucial for the success of Austin Moore's prosthesis (AMP) surgery to provide mechanical stability and allow bone grafts to consolidate.
2) Inadequate proximal fixation is one of the primary reasons for painful failure of AMP, which can result in prosthesis subsidence, loosening, and loss of alignment.
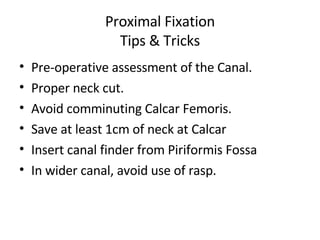
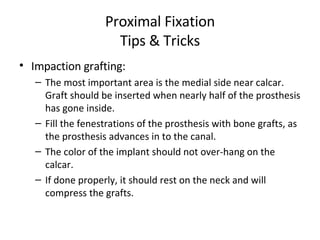
3) Achieving good proximal fixation requires careful pre-operative planning, preservation of femoral neck bone stock, impaction grafting of the proximal area, and selection of an appropriately sized implant.