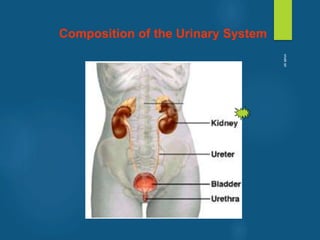
The document provides an overview of the urinary system, including its anatomy and functions. Some key points:
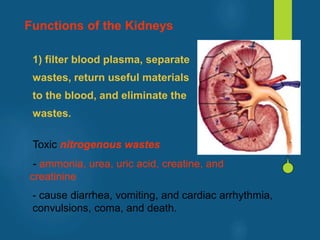
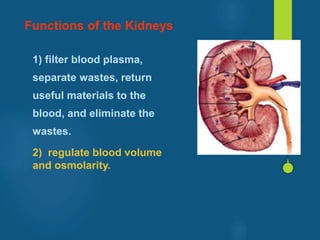
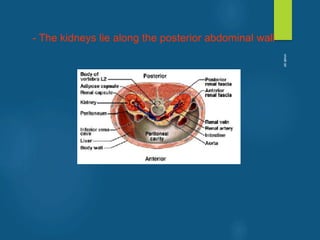
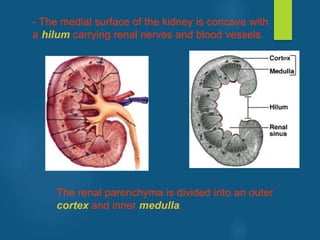
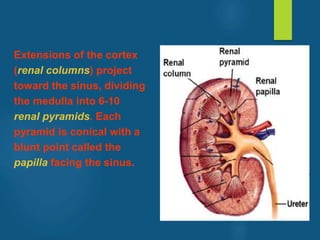
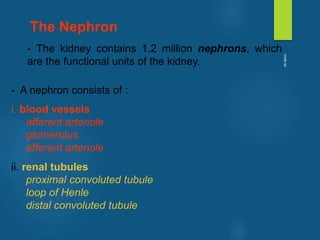
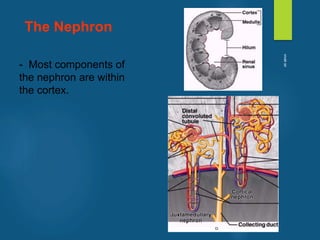
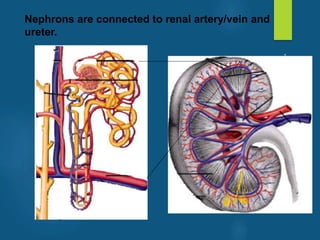
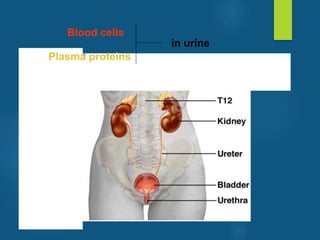
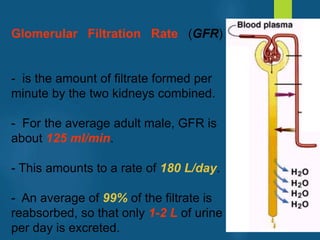
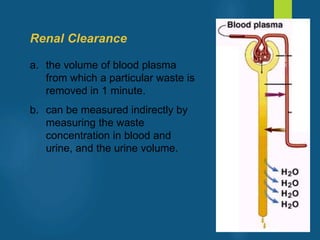
- The kidneys filter blood to remove waste and regulate fluid balance. Each kidney contains around 1 million nephrons, the functional units that filter blood into urine.
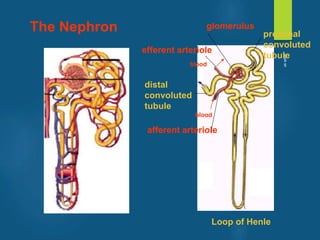
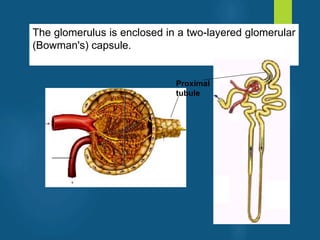
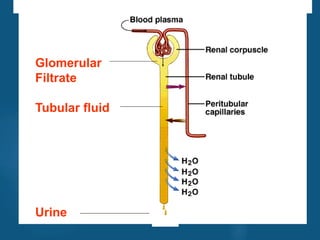
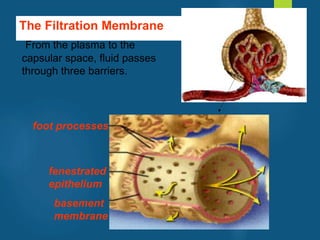
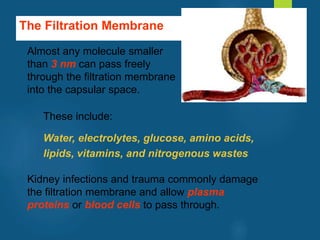
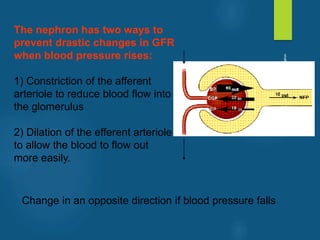
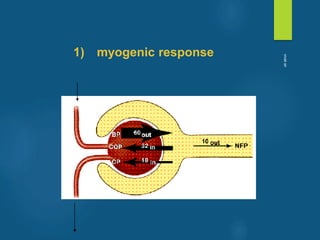
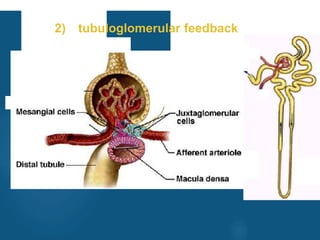
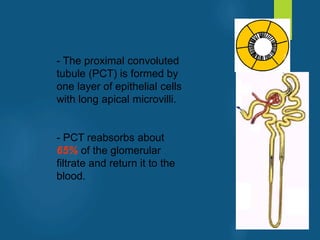
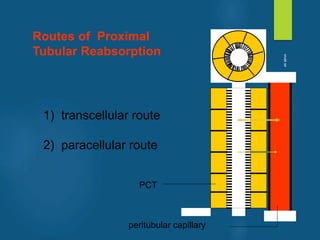
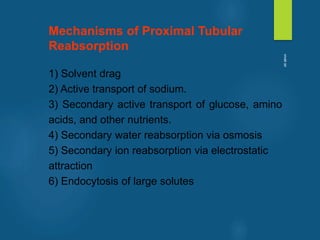
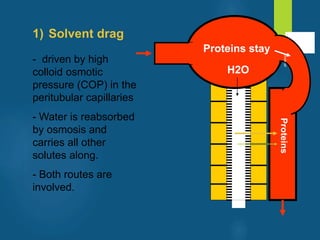
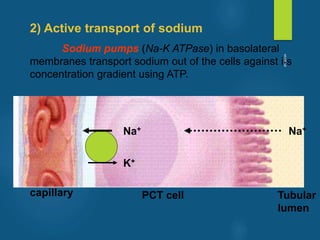
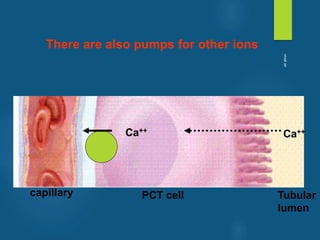
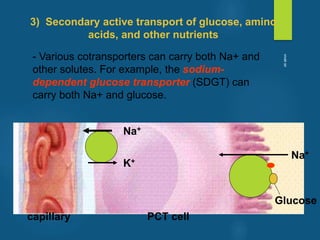
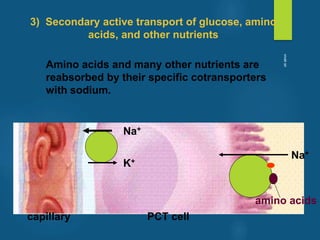
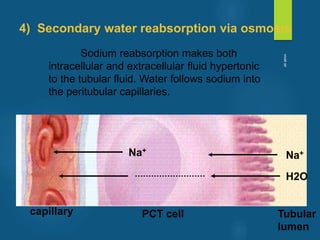
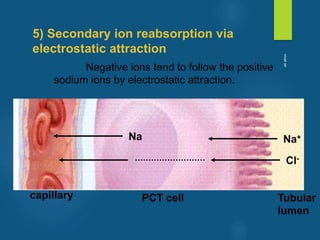
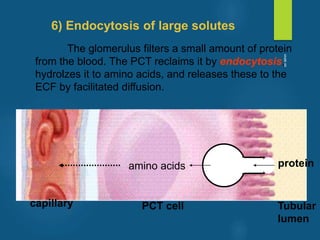
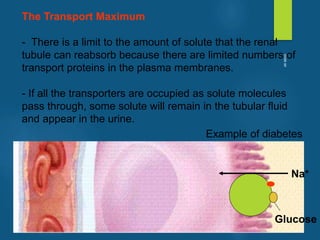
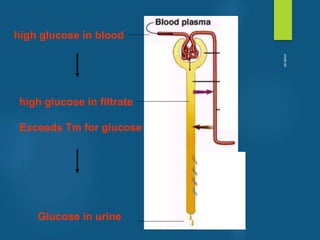
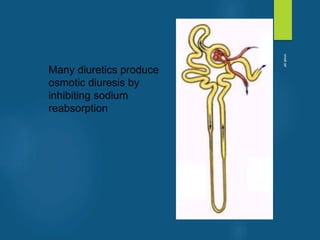
- The nephron is made up of blood vessels and tubules that work together to filter blood, reabsorb useful molecules, and secrete waste molecules into urine.
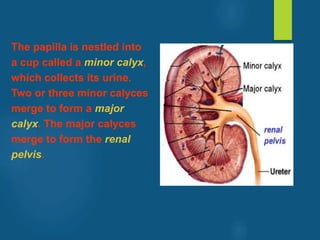
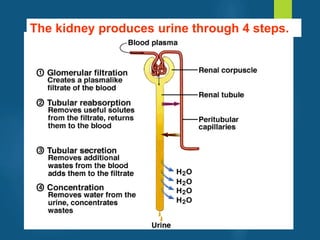
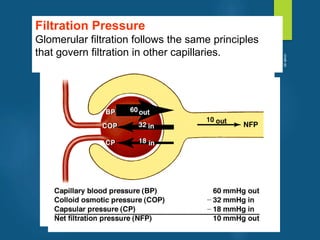
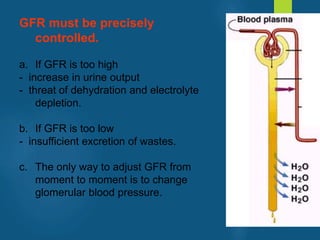
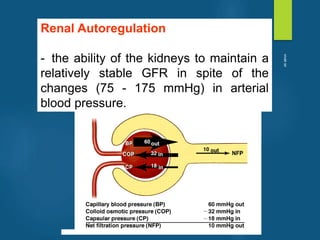
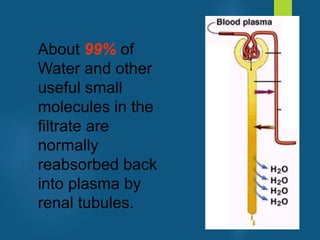
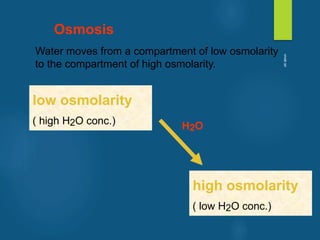
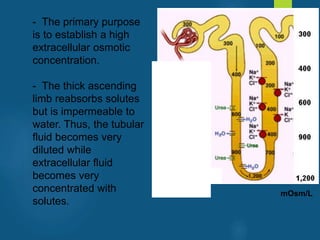
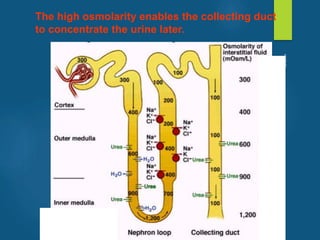
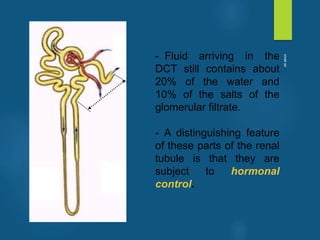
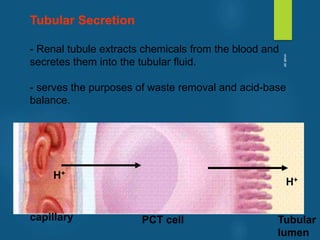
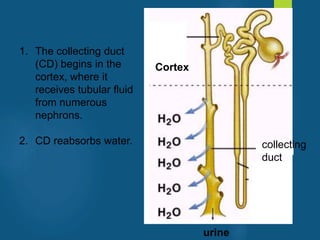
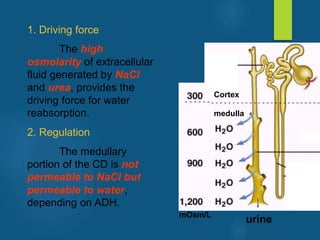
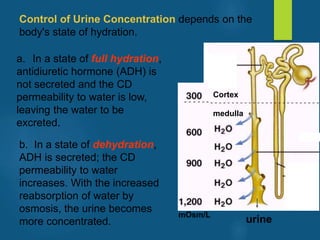
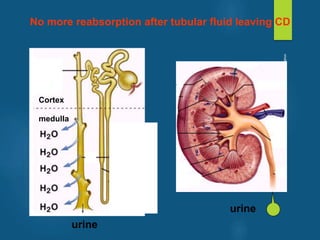
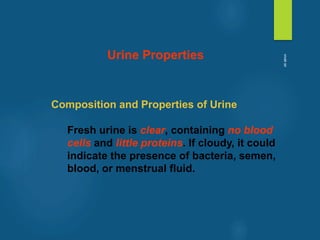
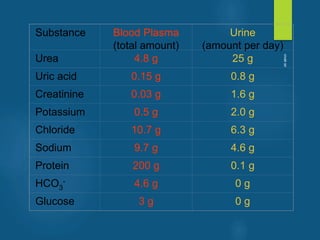
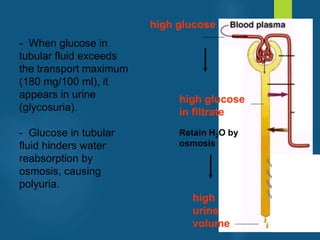
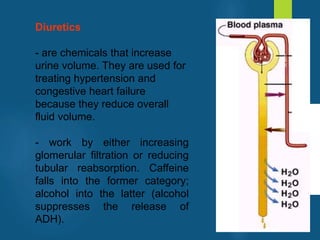
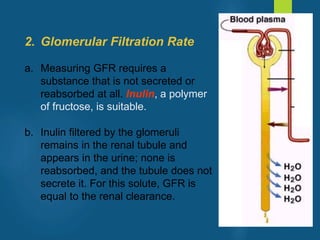
- Urine is formed in four steps - glomerular filtration, tubular reabsorption, tubular secretion, and concentration by the collecting duct. Nearly all the filtrate is reabsorbed except for waste products.
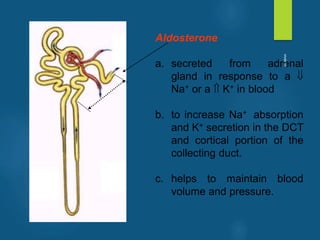
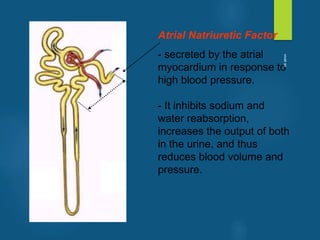
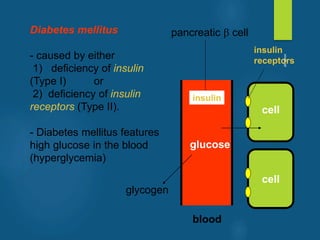
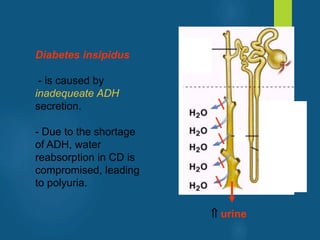
- Hormones