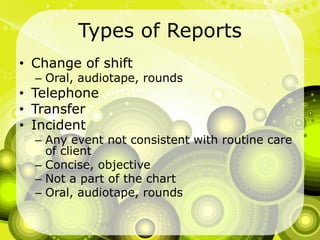
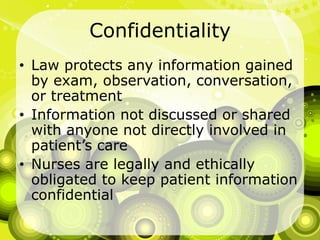
Documentation and recording communication with the healthcare team ensures quality of care and is required by regulatory agencies. It shows nursing actions, serves as a legal document, and involves summarizing activities, observations, and actions in an objective, non-judgmental manner through oral or written reports such as shift reports and reports to physicians. Various types of reports like change of shift reports, incident reports, and transfer reports must follow standards for documentation, including being legible, factual, complete, concise, timely, accurate, and organized according to guidelines in order to effectively communicate important patient information.