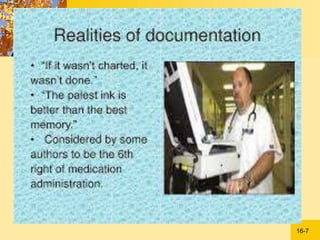
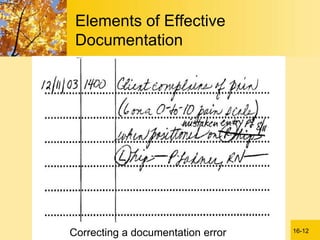
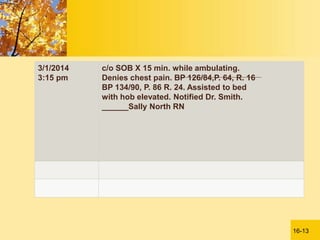
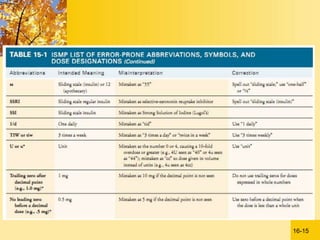
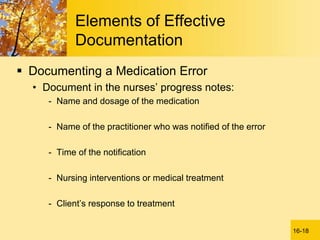
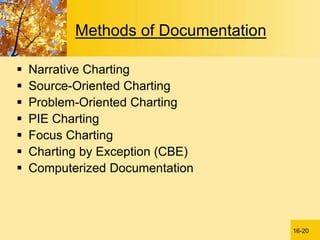
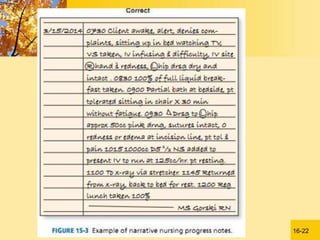
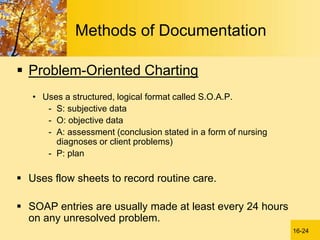
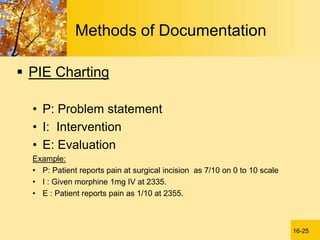
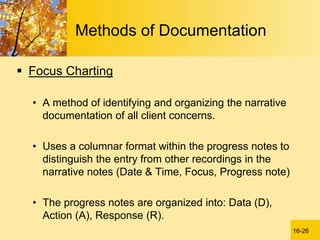
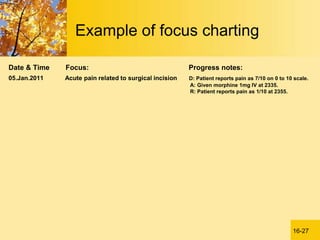
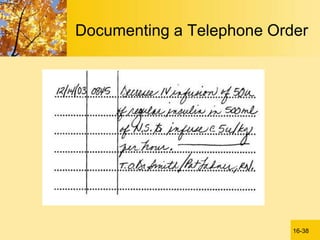
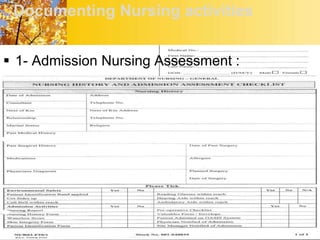
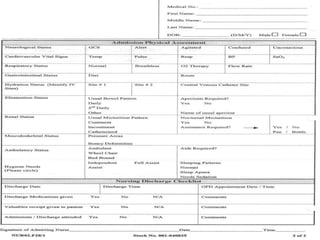
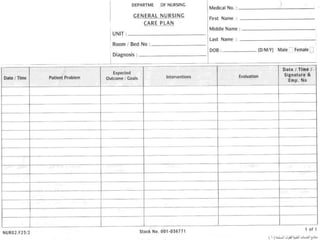
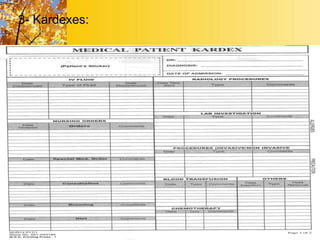
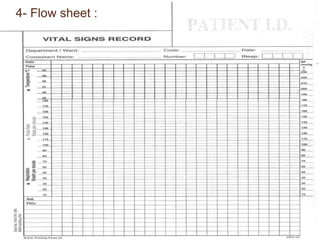
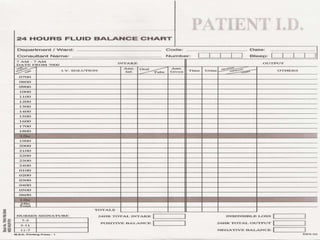
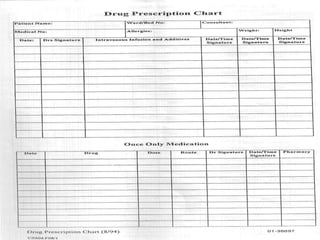
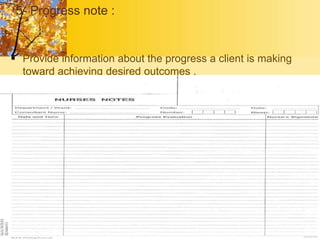
This document discusses documentation and reporting in healthcare. It explains that documentation is a major communication technique used to record interactions between providers and patients. Effective documentation includes using common vocabulary, legible writing, approved abbreviations, organization, accuracy, and maintaining confidentiality. Common documentation methods include narrative, problem-oriented, and computerized charting. Key documentation forms are kardexes for patient information, flow sheets to record vital signs and other data over time, and progress notes detailing care, interventions and outcomes. Regular reporting includes shift changes, rounds, incident reports, and communicating by telephone.