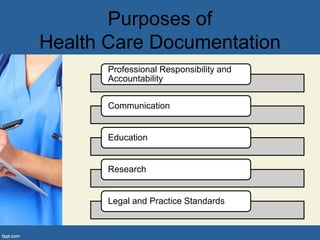
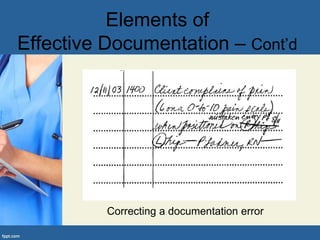
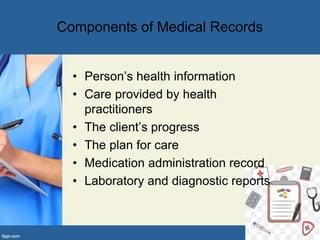
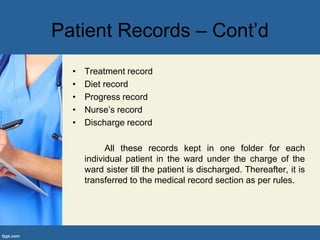
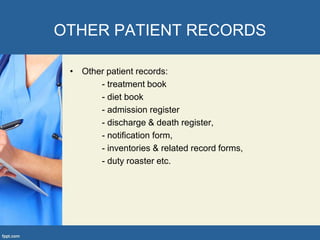
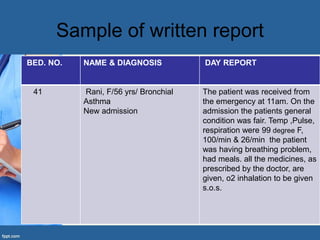
The document discusses the importance of effective documentation in healthcare, detailing its role in communication, legal accountability, and professional standards. It outlines various methods of documentation, such as narrative and problem-oriented charting, as well as key elements like accuracy, confidentiality, and correction of errors. Additionally, it highlights the different types of patient records and the significance of thorough reporting to ensure quality patient care.