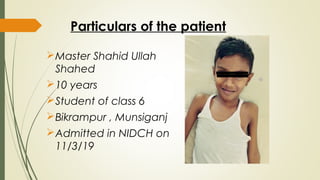
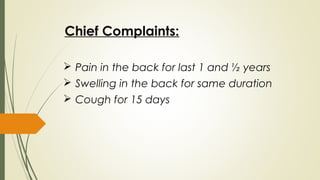
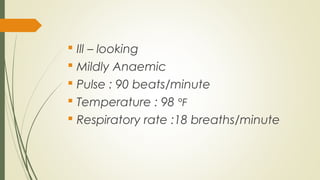
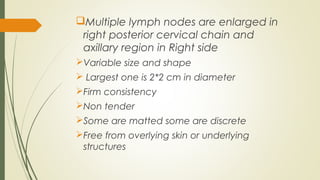
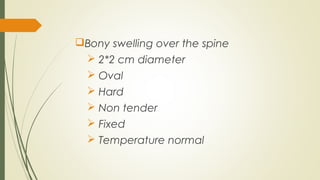
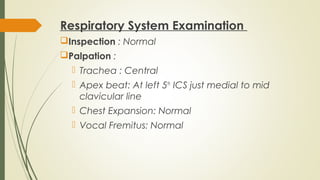
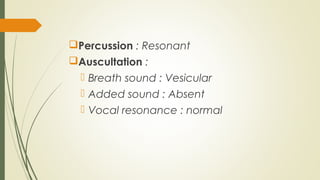
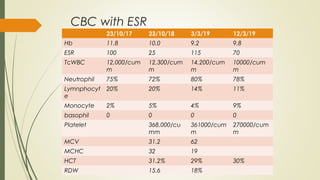
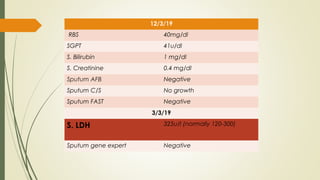
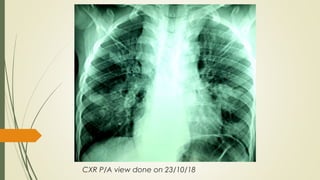
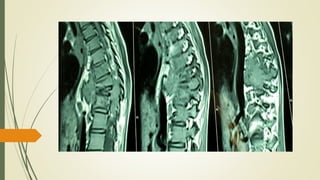
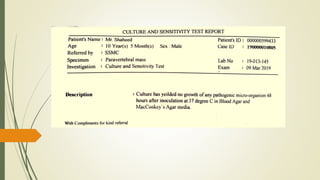
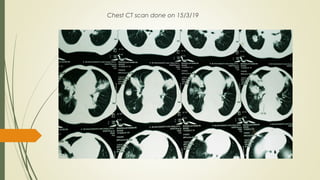
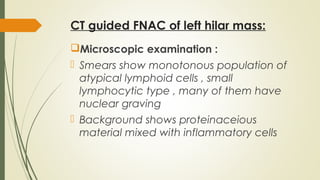
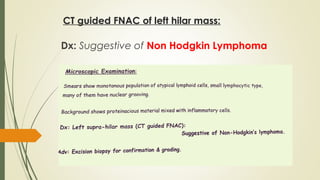
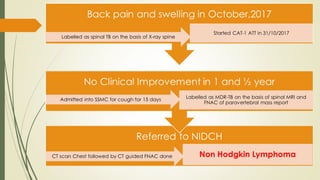
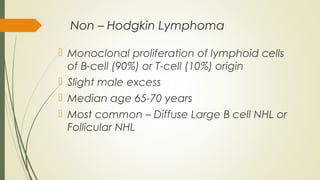
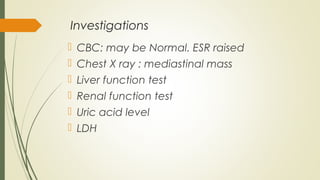
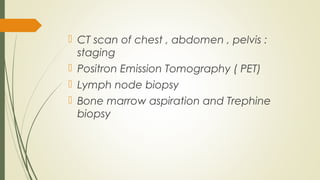
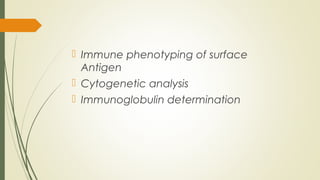
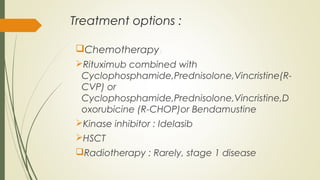
This document describes the case of a 10-year-old boy who presented with back pain and swelling for 1.5 years. Initial x-rays led to a diagnosis of spinal tuberculosis, but anti-tuberculosis treatment did not improve his condition. He then developed a cough. Further investigations including CT scans and biopsies revealed non-Hodgkin lymphoma with lymph node and lung involvement. Non-Hodgkin lymphoma can mimic other conditions at presentation and this case illustrates the importance of thorough investigation and follow-up given lack of response to initial treatment.