Cardio myopathy
- 2. INTRODUCTION Cardiomyopathies (CMPs) are primary disorders of myocardial structure and function in the absence of coronary artery disease, hypertension, valvular disease, and congenital heart disease. Knowledge of the incidence and prevalence of CMPs may help clinicians to compare their observations in clinical practice with expected cases per person-year and to avoid under- reporting in clinical context. Currently, available estimates of prevalence and incidence of CMPs are based on clinical data, collected with a wide variability in population-source, and before the genetic testing evolved as a standard diagnostic tool. This review focuses on the epidemiology of CMPs in subjects aged between 18 and 55 years. A structured up-to-date diagnostic flow-chart for CMPs diagnosis and assessment is proposed to avoid misdiagnosis of CMPs in the young populationThe prevalence of dilated cardiomyopathy (DCM) is approximately 1/250 (0.4%), of hypertrophic cardiomyopathy (HCM) is approximately 1/500 (0.2%) and of arrhythmogenic right ventricular cardiomyopathy (ARVC) is approximately 1/5,000 (0.02%)
- 3. DEFINITION OF CARDIO MYOPATHY Cardiomyopathy refers to diseases of the heart muscle. In cardiomyopathy, the heart muscle becomes enlarged, thick, or rigid. In rare cases, the muscle tissue in the heart is replaced with scar tissue.
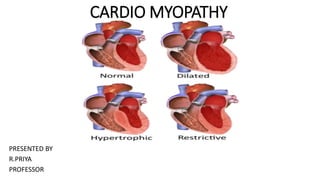
- 4. TYPES Hypertrophic Cardiomyopathy Dilated Cardiomyopathy Restrictive Cardiomyopathy Arrhythmogenic Right Ventricular Dysplasia Takotsubo cardiomyopathy Stress cardiomyopathy
- 5. CARDIOMYOPATHY Hypertrophic cardiomyopathy happens when the heart muscle enlarges and thickens without an obvious cause. Usually the ventricles, the lower chambers of the heart, and septum (the wall that separates the left and right side of the heart) thicken. The thickened areas create narrowing or blockages in the ventricles, making it harder for the heart to pump blood. Hypertrophic cardiomyopathy also can cause stiffness of the ventricles, changes in the mitral valve, and cellular changes in the heart tissue.Hypertrophic cardiomyopathy is very common and can affect people of any age. Hypertrophic cardiomyopathy affects men and women equally, and about 1 out of every 500 people has the disease. Other name of HCM is symmetric septal hypertrophy; idiopathic hypertrophic subaortic stenosis, hypertrophic obstructive cardiomyopathy
- 6. TYPES OF HCM Different types of HCM are described according to where in the heart the thickened area of muscle is. This also affects what symptoms someone might experience and what treatment is needed. Apical hypertrophy – the thickened area is at the bottom (apex) of the heart. This usually reduces the volume of the ventricle. Symmetrical hypertrophy – the thickening affects the whole of the left ventricle, reducing its volume. This is sometimes called ‘concentric’ hypertrophy. Asymmetrical septal hypertrophy without obstruction – the thickening affects the heart’s septum. ‘Without obstruction’ means that the thickening doesn’t affect or restrict the flow of blood leaving the heart. Asymmetrical septal hypertrophy with obstruction – the thickening affects the heart’s septum. However, unlike the type above, the thickened area causes an obstruction that affects the flow of blood leaving the heart. When this happens, the ventricle has to work harder to pump out blood. The mitral valve can also be affected and is unable to close properly. This means that blood leaks back into the atrium (called mitral regurgitation) which can cause a murmur (sound that can be heard through a stethoscope).
- 7. CAUSES OF HCM Genetics HCM is typically an inherited condition. Defective genes can cause your heart muscle to thicken. You have a 50 percent chance of inheriting one of these genes if one of your parents is affected by HCM. Hypertension
- 9. SIGNS AND SYMPTOMS OF HCM • Chest pain, especially during exercise • Fainting, especially during or just after exercise or exertion • Heart murmur, which a doctor might detect while listening to your heart • Sensation of rapid, fluttering or pounding heartbeats (palpitations) • Shortness of breath, especially during exercise
- 10. MANAGEMENT OF HCM •Beta blockers such as metoprolol (Lopressor, Toprol-XL), propranolol (Inderal, Innopran XL) or atenolol (Tenormin) •Calcium channel blockers such as verapamil (Verelan, Calan SR,) or diltiazem (Cardizem, Tiazac) •Heart rhythm drugs such as amiodarone (Pacerone) or disopyramide (Norpace) •Blood thinners such as warfarin (Coumadin, Jantoven), dabigatran (Pradaxa), rivaroxaban (Xarelto) or apixaban (Eliquis) to prevent blood clots if you have atrial fibrillation
- 11. SURGICAL MANAGEMENT Septal myectomy. This open-heart surgery may be recommended if medications do not improve your symptoms. It involves removing part of the thickened, overgrown wall (septum) between the heart chambers. Septal myectomy helps improve blood flow out of the heart and reduces backward flow of blood through the mitral valve (mitral regurgitation). The surgery may be done using different approaches, depending on the location of the thickened heart muscle. In one type, called apical myectomy, surgeons remove thickened heart muscle from near the tip of the heart. Sometimes the mitral valve is repaired at the same time. Septal ablation. This procedure destroys the thickened heart muscle with alcohol. The alcohol is injected through a long, thin tube (catheter) into the artery supplying blood to that area. Possible complications include disruption of the heart's electrical system (heart block), which requires implantation of a pacemaker. Implantable cardioverter-defibrillator (ICD). An ICD is a small device that continuously monitors your heartbeat. It's implanted in your chest like a pacemaker. If a life-threatening arrhythmia occurs, the ICD delivers precisely calibrated electrical shocks to restore a normal heart rhythm. ICD has been shown to help prevent sudden cardiac death, which occurs in a small number of people with hypertrophic cardiomyopathy.
- 12. DILATED CARDIOMYOPATHY Dilated cardiomyopathy develops when the ventricles enlarge and weaken. The condition usually starts in the left ventricle and over time can affect the right ventricle. The weakened chambers of the heart don’t pump effectively, causing the heart muscle to work harder. Over time, the heart loses the ability to pump blood effectively. Dilated cardiomyopathy can lead to heart failure, heart valve disease, irregular heart rate, and blood clots in the heart. Other names OF DCM IS Congestive cardiomyopathy, idiopathic cardiomyopathy, primary cardiomyopath
- 13. CAUSES /RISK FACTOR OF DCM It may be difficult to determine the cause of dilated cardiomyopathy. The condition often runs in families (is inherited). However, many things can cause the left ventricle to dilate and weaken, including: •Diabetes •Obesity •Heart rhythm problems (arrhythmias) •High blood pressure (hypertension) •Complications of late-stage pregnancy •Excessive iron in your heart and other organs (hemochromatosis) •Certain infections Other possible causes of dilated cardiomyopathy include: •Alcohol abuse •Use of certain cancer medications •Use of illegal drugs, such as cocaine or amphetamines •Exposure to toxins, such as lead, mercury and cobalt Risk factors Risk factors for dilated cardiomyopathy include: •Long-term high blood pressure •Family history of dilated cardiomyopathy, heart failure or sudden cardiac arrestACTOR •Inflammation of the heart muscle from immune system disorders, such as lupus •Damage to the heart muscle from certain diseases, such as hemochromatosis •Neuromuscular disorders, such as muscular dystrophy
- 15. SIGNS AND SYMPTOMS OF DCM •Shortness of breath with exertion. This may get worse so that you have shortness of breath when at rest. •Shortness of breath when lying flat •Sudden shortness of breath that wakes you up at night •Tiredness (fatigue) •Less able to be active and exercise •Swelling in the legs and other areas •Fainting •Weakness or lightheadedness •Cough •Heart rhythms problems
- 16. DIAGNOSTIC EVALUATION OF DCM •Echocardiogram, to look at blood flow in the heart, the size of the heart chambers, and heart motion using ultrasound •Electrocardiogram (ECG) to check the heart rhythm •Continuous portable ECG monitoring to check heart rhythms away from the healthcare provider’s office •Chest X-ray to see the heart anatomy •Exercise testing to see how your heart does during exercise Depending on your health history, you may have other tests such as: •Cardiac stress testing to look for blood flow problems to the heart •Blood work to check for various problems or infections such as HIV or Lyme disease •Blood work to check for autoimmune diseases •Cardiac MRI to further check the heart anatomy and coronary arteries •Heart biopsy to look at the heart in more detail •Cardiac catheterization with coronary angiography to look at the arteries •Genetic testing
- 17. MANAGEMENT O F DCM Angiotensin converting enzyme inhibitors lisinopril (32.5–35 mg) are as well tolerated as low doses (2.5–5 mg), β Blockers; bisoprolol, metoprolol Spironolactone; Anticoagulants; warfarin. Immunomodulation/immunosuppression; Immunosuppression is also a rather indiscriminate weapon, as it may suppress potentially beneficial immune responses such as neutralising antibody production in patients with chronic viral myocarditis. New approaches to the diagnosis of chronic myocarditis and the treatment of inflammatory cardiomyopathy should improve this situation. There are already interesting preliminary data suggesting that high dose immunoglobulin and immunoadsorption may result in short term improvement in left ventricular performance in patients with dilated and peripartum cardiomyopathy.
- 18. MANAGEMENT O F DCM Partial left ventriculectomy (“Batista” procedure) Partial left ventriculectomy is based on the hypothesis that as wall tension is related to left ventricular diameter (Laplace's law), reducing the left ventricular size by excision of a portion of its circumference should reduce wall stress and improve ventricular haemodynamics. In the best centres results from this intervention were initially remarkably good given the nature of the procedure. It is clear, however, that even with careful patient selection many patients survive only with the benefit of left ventricular assist devices and subsequent transplantation. Late sudden death is also described in a proportion of survivors. The difficulties associated with patient selection and subsequent postoperative care suggest that, at best, this form of treatment will be confined to a very small number of experienced centres. Left ventricular assist devices Left ventricular assist devices (LVADs) have recently received approval from the US Food and Drug Administration for use in patients with end stage heart failure as a bridge to cardiac transplantation. Experience in patients with IDC suggests that LVAD treatment can result in an apparent improvement in left ventricular function that may persist when the device is removed. However, there are as yet no reliable markers that distinguish the minority of patients that sustain useful recovery from the majority that deteriorate following explantation of the device. Technical advances in LVAD design now raise the possibility of using these devices as an alternative to transplantation in patients who are not transplant candidates. This mode of treatment is currently being evaluated in the REMATCH study, which if positive will have substantial clinical and resource implications for centres managing advanced heart failure. Multisite ventricular pacing Many patients with advanced IDC have abnormal left ventricular activation that in turn results in prolonged and incoordinate ventricular relaxation. In some patients ventricular conduction delay is also associated with prolongation of atrioventricular conduction, resulting in a loss of atrioventricular synchrony and a predisposition to prolonged functional mitral regurgitation. Dual chamber pacing has been advocated as a method for restoring AV synchrony and improving left ventricular coordination in patients with severe congestive heart failure. Although initially favourable haemodynamic results using conventional right ventricular pacing were not confirmed by later studies, there has been a more consistent response in studies that have used biventricular pacing, the outcome depending critically on the native QRS duration and the paced AV delay. Patients should be considered for biventricular pacing if they have QRS duration greater than 150 ms, PR interval prolongation, and symptoms refractory to conventional medical treatment.
- 19. COMPLICATION OF DCM •Heart failure. If you have dilated cardiomyopathy, your heart might not be able to supply your body with the blood it needs to work properly, leading to heart failure. Fluid can build up in the lungs, abdomen, legs, ankles and feet. •Heart valve regurgitation. Enlargement of the left ventricle may make it harder for your heart valves to close, causing a backward flow of blood and making your heart pump less effectively. •Heart rhythm problems. Changes in your heart's structure and changes in pressure on your heart's chambers can lead to the development of abnormal heart rhythms (arrhythmias). •Sudden cardiac arrest. Dilated cardiomyopathy can cause your heart to suddenly stop beating. •Blood clots (emboli). Pooling of blood in the left ventricle can lead to blood clots, which may enter the bloodstream and cut off the blood supply to vital organs. These blood clots can cause stroke, heart attack or damage to other organs. Arrhythmias can also cause blood clots.
- 20. PREVENTION OF DCM •Don't smoke. •Don't drink alcohol, or drink in moderation. •Don't use cocaine or other illegal drugs. •Eat a healthy diet that is low in salt (sodium). •Maintain a healthy weight. •Follow an exercise program recommended by your doctor. •Get enough sleep and rest. •Manage stress.
- 21. DEFINITION OF RCM Restrictive cardiomyopathy tends to affect older adults. The heart's ventricles become rigid because abnormal tissue, such as scar tissue, replaces the normal heart muscle. Consequently, the ventricles can't relax normally and fill with blood, and the atria become enlarged. Blood flow in the heart is reduced over time. This can lead to problems such as heart failure or arrhythmias. •OTHER name of RVM is •Idiopathic restrictive cardiomyopathy •Infiltrative cardiomyopathy
- 22. CAUSES OF RCM •Hemochromatosis. (A disease in which too much iron builds up in your body. The extra iron is toxic to the body and can damage the organs, including the heart.) •Sarcoidosis. (A disease that causes inflammation and can affect the body's organs. Researchers believe that an abnormal immune response may cause sarcoidosis. The abnormal response causes tiny lumps of cells to form in the body's organs, including the heart.) •Amyloidosis. (A disease in which abnormal proteins build up in the body's organs, including the heart.) Amyloid light chain amyloidosis is a "protein misfolding disorder." It causes organs and tissues, including the heart, kidney, skin, stomach, small and large intestines, nerves and liver, to thicken and eventually lose function. •Connective tissue disorders •Some cancer treatments, such as radiation and chemotherapy Drugs (serotonin, methysergide, ergotamine, mercurial agents, busulfan) Radiation diopathic
- 24. SIGNS AND SYMPTOMS OF RCM •Shortness of breath (at first with exercise; but over time it occurs at rest) •Fatigue (feeling overly tired) •Inability to exercise •Swelling of the legs and feet •Weight gain •Nausea, bloating, and poor appetite (related to fluid retention) •Palpitations (fluttering in the chest due to abnormal heart rhythms) Less common symptoms: •Fainting (caused by irregular heart rhythms, abnormal responses of the blood vessels during exercise, or no cause may be found) •Chest pain or pressure (occurs usually with exercise or physical activity, but can also occur with rest or after meals)
- 25. DIAGNOSTIC EVALUATION OF RCM •Electrocardiogram (ECG), to check the heart rhythm •Continuous portable ECG monitoring, to look at heart rhythms while you are away from the healthcare provider’s office •Chest X-ray, to see the heart size and anatomy •Blood tests, to help assess the type of RCM •Echocardiogram, to examine blood flow in the heart and how well the heart pumps blood to the body •Exercise testing, to see how your heart does during exercise •Cardiac MRI, to further look at heart anatomy and coronary arteries •Heart biopsy, to look at a small tissue sample from the heart in more detail •Cardiac catheterization with coronary angiography. This looks at the arteries in special cases, as well as measures pressures within the heart.
- 26. MANAGEMENT OF RCM •Water pills (diuretics) to reduce swelling •Medicine such as rate-lowering calcium channel blockers or beta-blockers to reduce the heart’s workload and increase its efficiency •Medicine such as ACE inhibitors to help the heart pump better •Blood thinners (anticoagulants) to prevent blood clots if you have certain abnormal heart rhythms •Medicine to help prevent abnormal heart rhythms •Lifestyle changes, such as cutting back on salt to reduce swelling •Heart transplant. This may be considered in advanced cases.
- 27. DEFINITION ARVC Arrhythmogenic right ventricular cardiomyopathy, or ARVC, is a type of cardiomyopathy that affects the ventricles (lower pumping chambers) of the heart and causes arrhythmias (abnormal heart rhythms). It affects the right ventricle, and often also affects the left ventricle. For this reason it is sometimes called arrhythmic cardiomyopathy (as the main symptoms are arrhythmias). It doesn’t affect the atria (upper chambers) of the heart.
- 28. CAUSES OF ARVD/C Arrhythmogenic right ventricular dysplasia/cardiomyopathy (ARVD/C) is caused by abnormalities of structures that connect heart muscle cells together. These structures are known as desmosomes. ARVC is often ‘autosomal dominant’. This means that the mutated gene is found on one of the non-sex chromosomes (called the autosomes). A child of an affected parent will have a 50% chance of inheriting the gene mutation. In some cases it is ‘recessive’ (and it therefore only develops into the condition if both parents pass on the gene).
- 30. SIGNS AND SYMPTOMS OF ARVC •Palpitations (feeling your heart beating too fast, too hard or like it is ‘fluttering’) – this is caused by arrhythmias (when the electrical messages which control the heart’s rhythm are disrupted). •Light-headedness and fainting (loss of consciousness) – reduced oxygen levels or blood flow to the brain, due to arrhythmias, can cause light- headedness or dizziness and, in some cases, loss of consciousness. •Swollen legs, ankles and tummy – build-up of fluid in the tissues, because the heart isn’t pumping effectively, can cause swelling (called ‘oedema’). •Breathlessness (or dyspnoea) – fluid builds-up around the lungs, making it harder to breathe. Due to the effect of ARVC on the electrical signalling the in the heart, it often causes arrhythmias. As ARVC affects the electrical signalling the in the heart, it often causes arrhythmias. Arrhythmias Arrhythmias are caused by the disruption of the normal electrical signalling in the heart that controls the heart beat. This disruption causes a change in the heart’s rhythm, which means it beats too fast, too slow or erratically. Types of arrhythmias that can happen in ARVC include the following. •Atrial fibrillation (AF) – caused by disruption of the electrical messages that normally cause the heart muscle to contract. In AF the atria beat very quickly and are uncoordinated. This can make the flow of blood around the atrium ‘turbulent’, and the heart less efficient at pumping out blood. AF can cause palpitations and increase the risk of blood clots forming, which can increase the risk of a stroke. •Ventricular premature beats (VPB) – this is an extra heart beat that happens when electrical impulses start in one of the ventricles, and it contracts before it receives the normal signal via the atria. ARVC can sometimes cause an increase in the number and frequency of these extra beats. •Ventricular tachycardia (VT) – VT starts due to abnormal electrical activity in the ventricles, where the heart contracts abnormally quickly (over 100 beats per minute). It can lead to loss of consciousness. •Ventricular fibrillation (VF) – the contraction of the ventricles is uncoordinated, and they ‘quiver’ rather than contract normally, so blood is not pumped out of the heart effectively. This condition is life-threatening and requires urgent treatment with a defibrillator (see treatment below).
- 31. MANAGEMENT OF ARVC •ACE inhibitors (angiotensin-converting enzyme inhibitors) – relax the smooth muscle around the blood vessels to reduce the workload on the heart, and reduce the volume of the blood, making it easier for the heart to work. •Anti-arrhythmic medication – reduces abnormal heart rhythms and helps to control the normal rhythm. •Anticoagulants (blood thinners) – may be used in people with arrhythmias to reduce the risk of blood clots forming, which could lead to a stroke. •Angiotensin II Receptor Blockers (ARBs) – dilate (enlarge) the blood vessels which helps to reduce blood pressure and may be used if the person is not able to tolerate ACE inhibitors. •Beta-blockers – reduce the rate and force of the heart’s contraction, by reducing stimulation of adrenalin (which would normally make the heart beat faster). •Diuretics (water tablets) – reduce the build-up of fluid on the lungs or the ankles by encouraging the kidneys to get rid of water as urine. •Pacemaker – may be recommended for people who have heart block (which makes the heart rate slow down). Pacemakers control the electrical signalling of the heart to keep a normal heart rhythm. •Cardioversion – this is a when an electric shock is given to the heart to try and control arrhythmias, most commonly atrial fibrillation, and put the heart back into a normal rhythm. This is similar to what an ICD does (see below) but is a procedure done in hospital. •Catheter ablation – this uses radio waves to treat areas of the heart where the electrical pathways cause arrhythmias. It stops the transmission of electrical signals that affect the normal heart rhythm. •ICDs (implantable cardioverter defibrillator) – this may be recommended due to the risk of life-threatening arrhythmias. ICDs detect and correct any dangerous arrhythmias which could otherwise lead to a cardiac arrest.
- 32. DEFINITION OF TTS • Takotsubo cardiomyopathy or "Broken Heart Syndrome" is when the heart muscle becomes suddenly stunned or weakened. It mostly occurs following severe emotional or physical stress. The condition is temporary and most people recover within two moths. t is also known as stress cardiomyopathy, apical ballooning, or broken heart syndrome. Takotsubo cardiomyopathy most often affects women between the ages of 61 and 76 years. The condition commonly occurs immediately after experiencing extreme emotional or physical stress. Transient apical ballooning syndrome, apical ballooning cardiomyopathy, stress-induced cardiomyopathy, broken-heart syndromeTHESE ARE OTHER NAME OF TTS Schematic representation of takotsubo cardiomyopathy (A) compared to a normal heart (B) Specialty Cardiology
- 33. CAUSES OF TTS Events that could trigger takotsubo cardiomyopathy include: •the sudden death of a loved one •domestic abuse •natural disasters •a motor vehicle accident •a fierce argument •relationship conflicts •severe financial or gambling losses •being diagnosed with a medical condition •exhausting physical effort •surgery •acute medical illnesshead trauma •public speaking •extreme fright Cases of takotsubo cardiomyopathy have also been reported after cocaine use, excessive stimulant drug use, or during opiate withdrawal. People with certain mood disorders might be more likelyTrusted Source than others to develop takotsubo cardiomyopathy. Some instances of takotsubo cardiomyopathy have occurred after positive stressful events, such as winning the lottery or a surprise party. It is not understood why a specific stressful event will trigger this condition, but at a similar event may not do so at a different time. Also, experts do not yet know why it is primarily older women that have takotsubo cardiomyopathy. A drop in estrogen activity may be a contributing factor in older women.
- 34. SIGNS AND SYMPTOMS OF TTS • Chest pain and shortness of breath after severe stress (emotional or physical) • Electrocardiogram abnormalities that mimic those of a heart attack. • No evidence of coronary artery obstruction. • Movement abnormalities in the left ventricle. • Ballooning of the left ventricle.
- 35. MANAGEMENT OF TTS •ACE inhibitors to lower blood pressure (long term). •Beta blockers to slow the heart rate (short term). •Diuretics to decrease fluid buildup (short term). •Anti-anxiety medicines to manage stress. (These medications may be long term, if needed.) Depending on how much your heart muscle was weakened, your healthcare provider may also recommend cardiac rehabilitation. Managing your stress with yoga, meditation and other relaxation techniques can also be helpful. Ask your healthcare provider for information on these methods and possible programs and services available.
- 36. PREVENTION OF TTS There are no known treatments for preventing broken heart syndrome. However, learning stress management and problem-solving techniques can help improve physical and emotional stress. Engaging in relaxation techniques can also be helpful. Some examples include: •Practicing yoga, meditation, journaling, or mindfulness. •Taking a warm bath; lighting scented candles; and taking long, deep breaths and slowly exhaling. Depending on the source of your stress, there may be a support group you can join to talk about your stress and share coping skills with others who have had similar experiences. Seeking the help of a professional counselor might be considered too. In addition, managing physical or emotional stress can be helped by following general healthy habits too.These include: •Eating a healthy diet, such as the Dash diet or Mediterranean diet. •Getting regular exercise (at least five times a week for 30 minutes). •Getting seven to nine hours of sleep each night. •Spending time with others. •Keeping your medical appointments, for both follow up and preventive health screenings. Finding and treating any health problems early always leads to the best outcome for a long and healthy life. •Avoid – or better yet – stop unhealthy choices such as smoking, illicit drug use, and alcohol abuse.