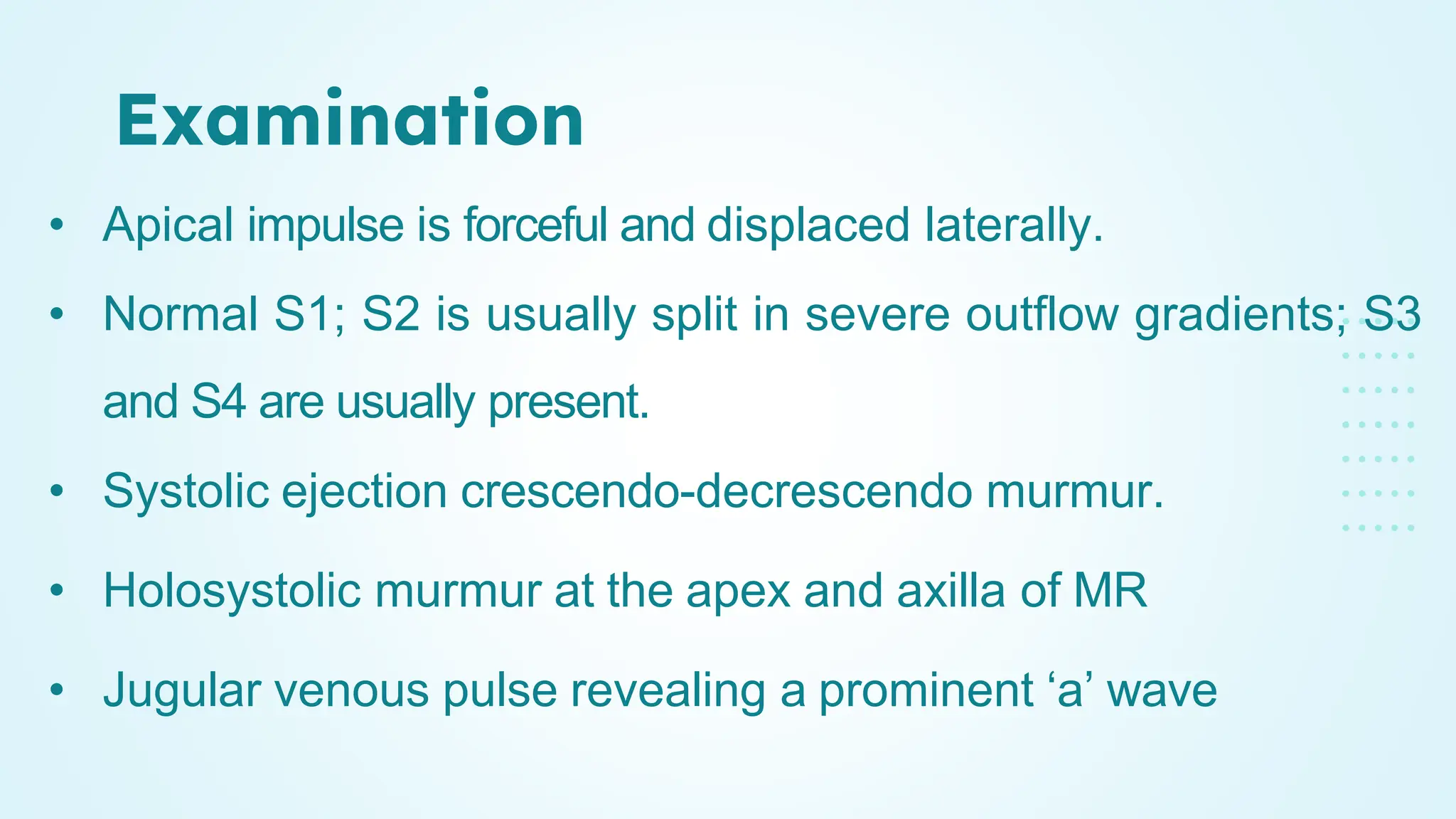
The document provides an in-depth overview of cardiomyopathies, detailing their definitions, classifications, pathophysiology, symptoms, diagnostics, and treatment options. It covers specific types like dilated, hypertrophic, and restrictive cardiomyopathies, discussing underlying causes and management strategies, including lifestyle changes, medications, and surgical interventions. The text emphasizes the importance of regular monitoring and tailored approaches to the patient's individual condition.