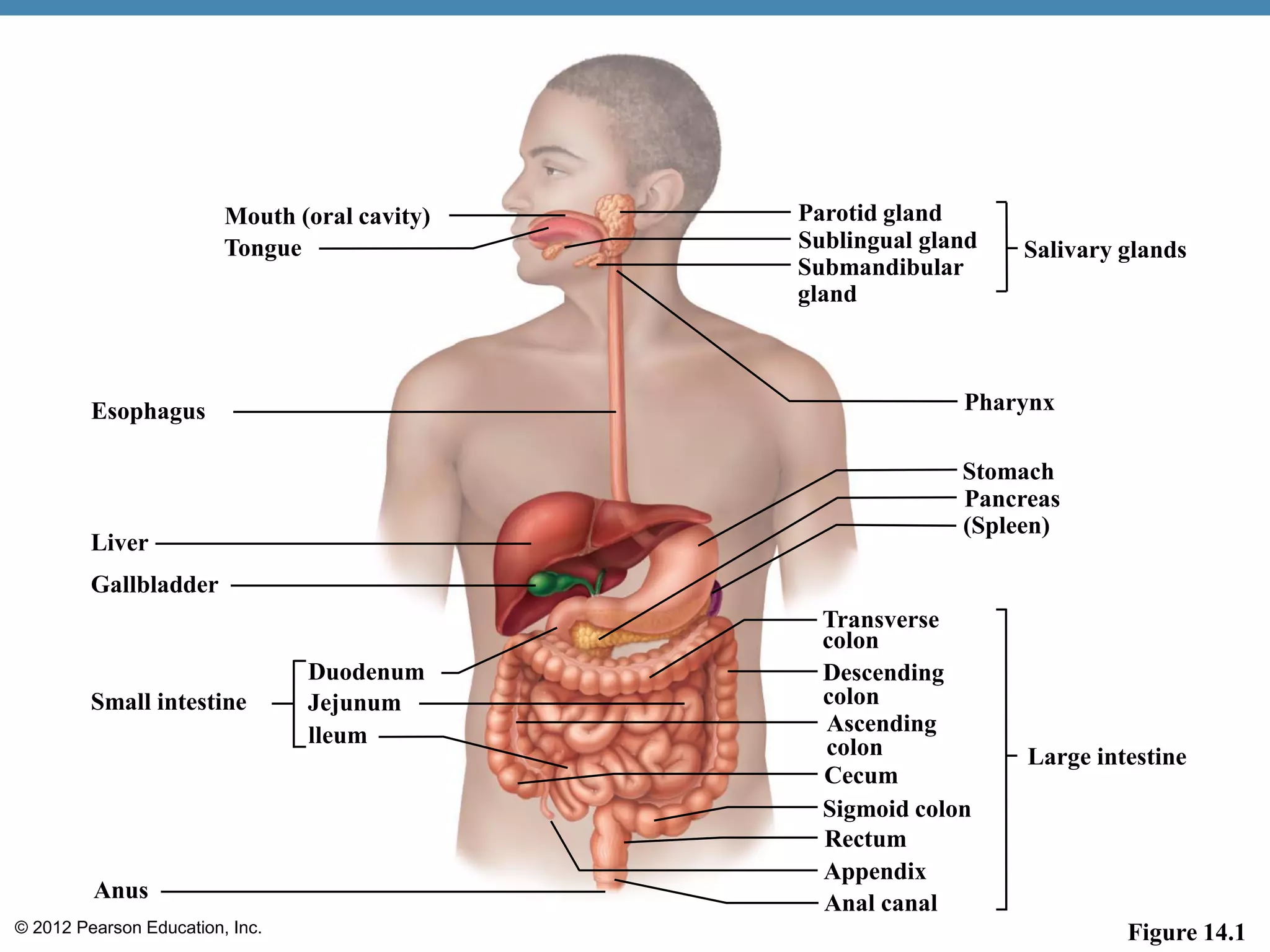
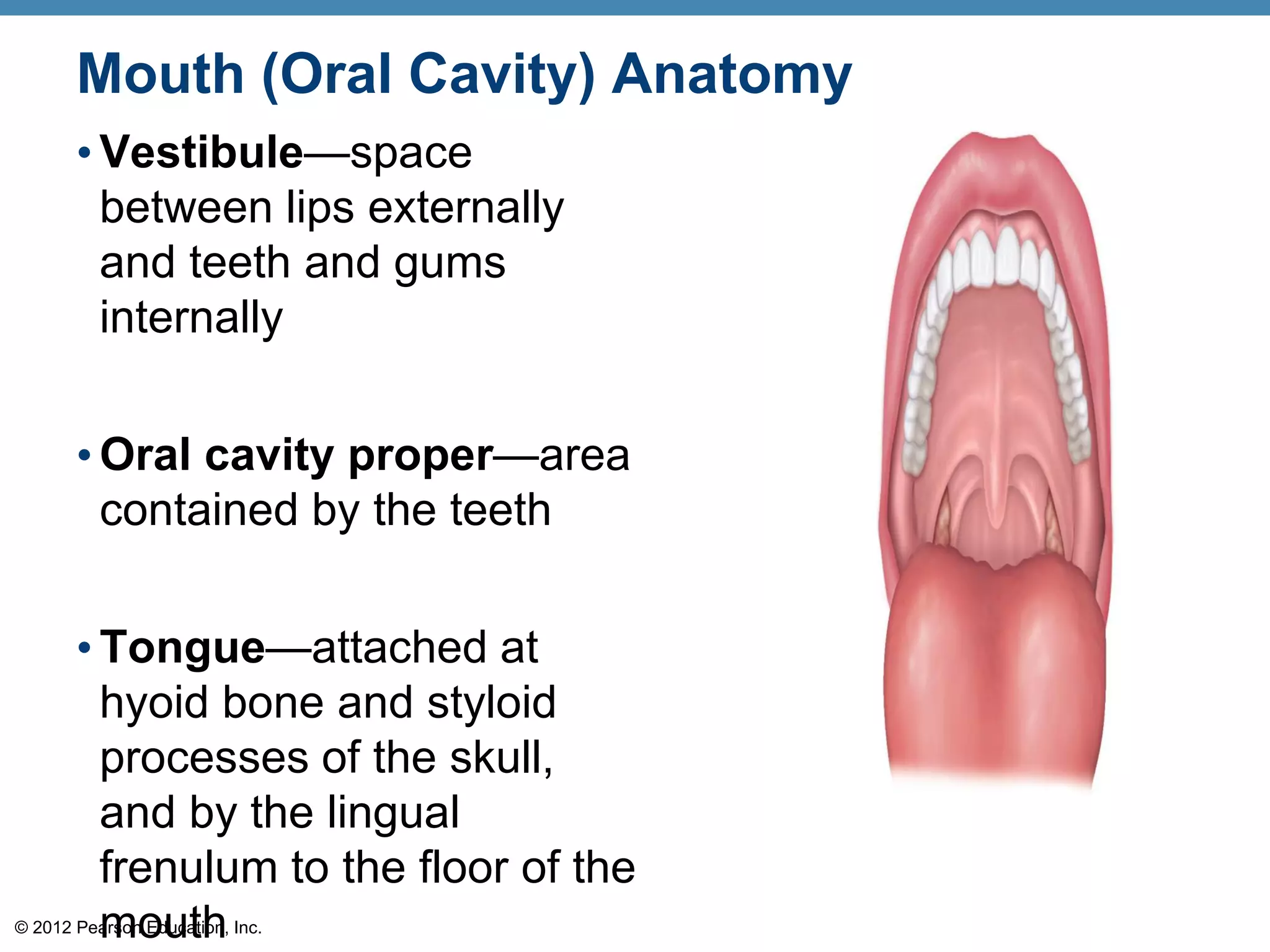
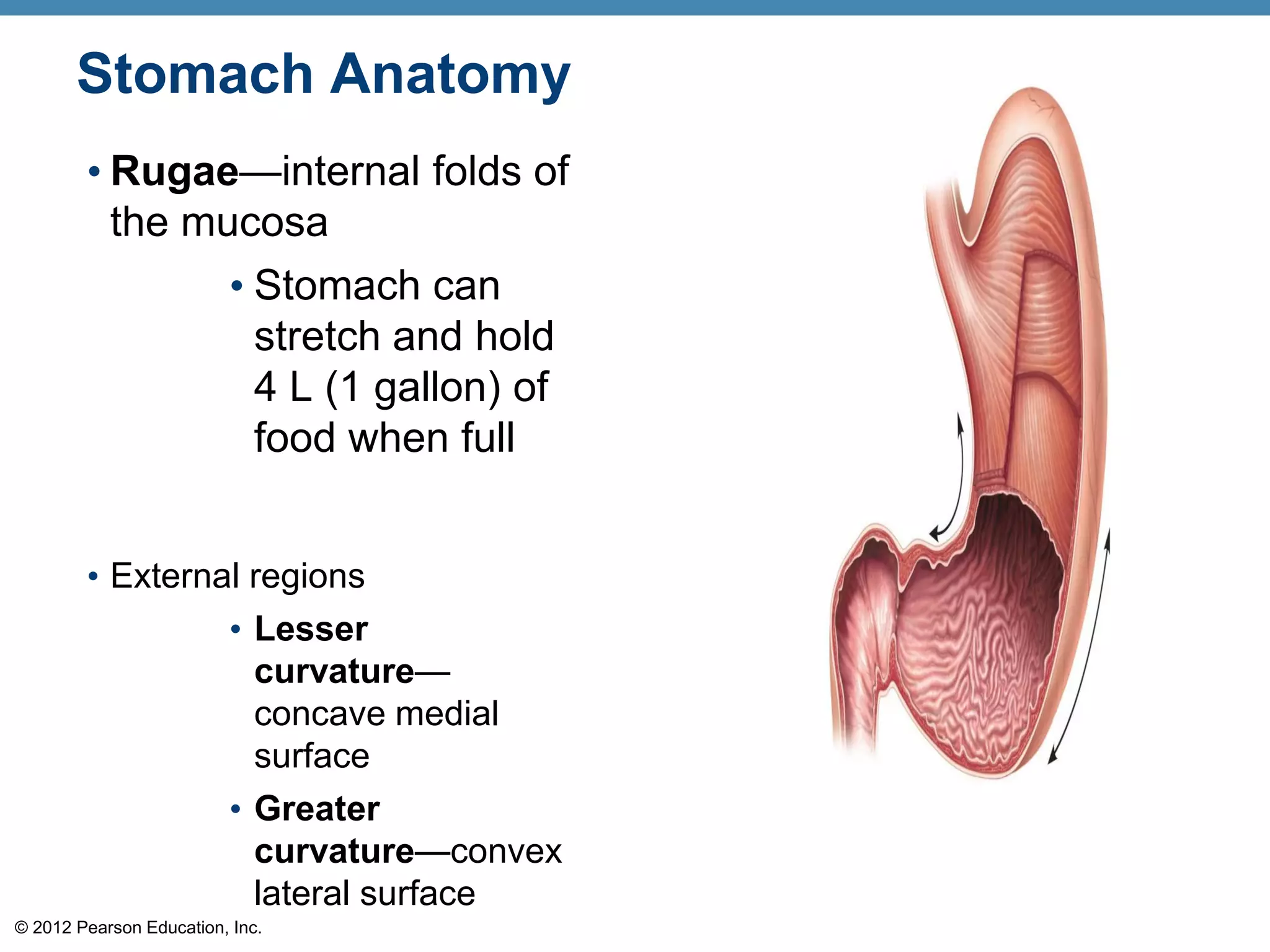
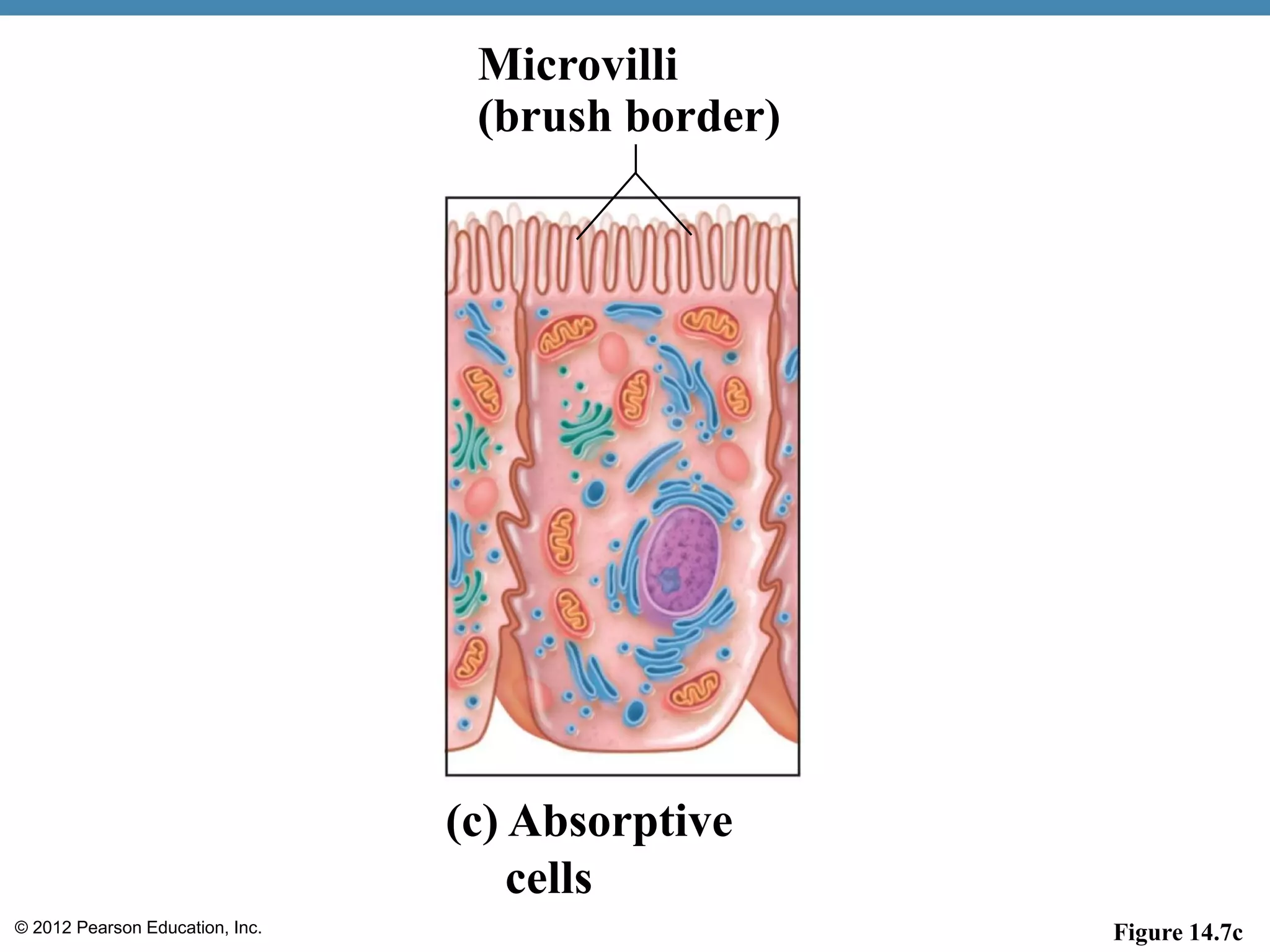
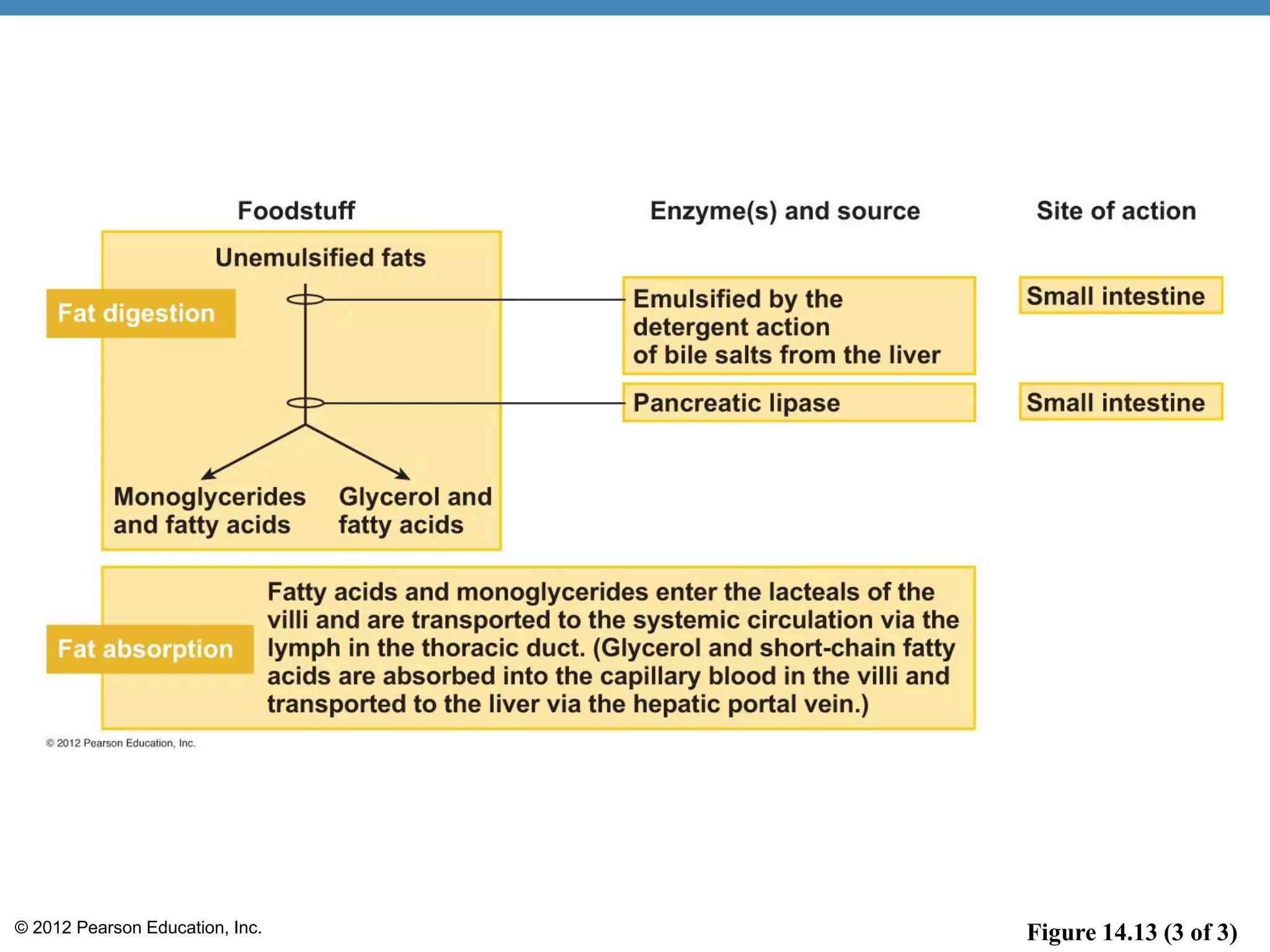
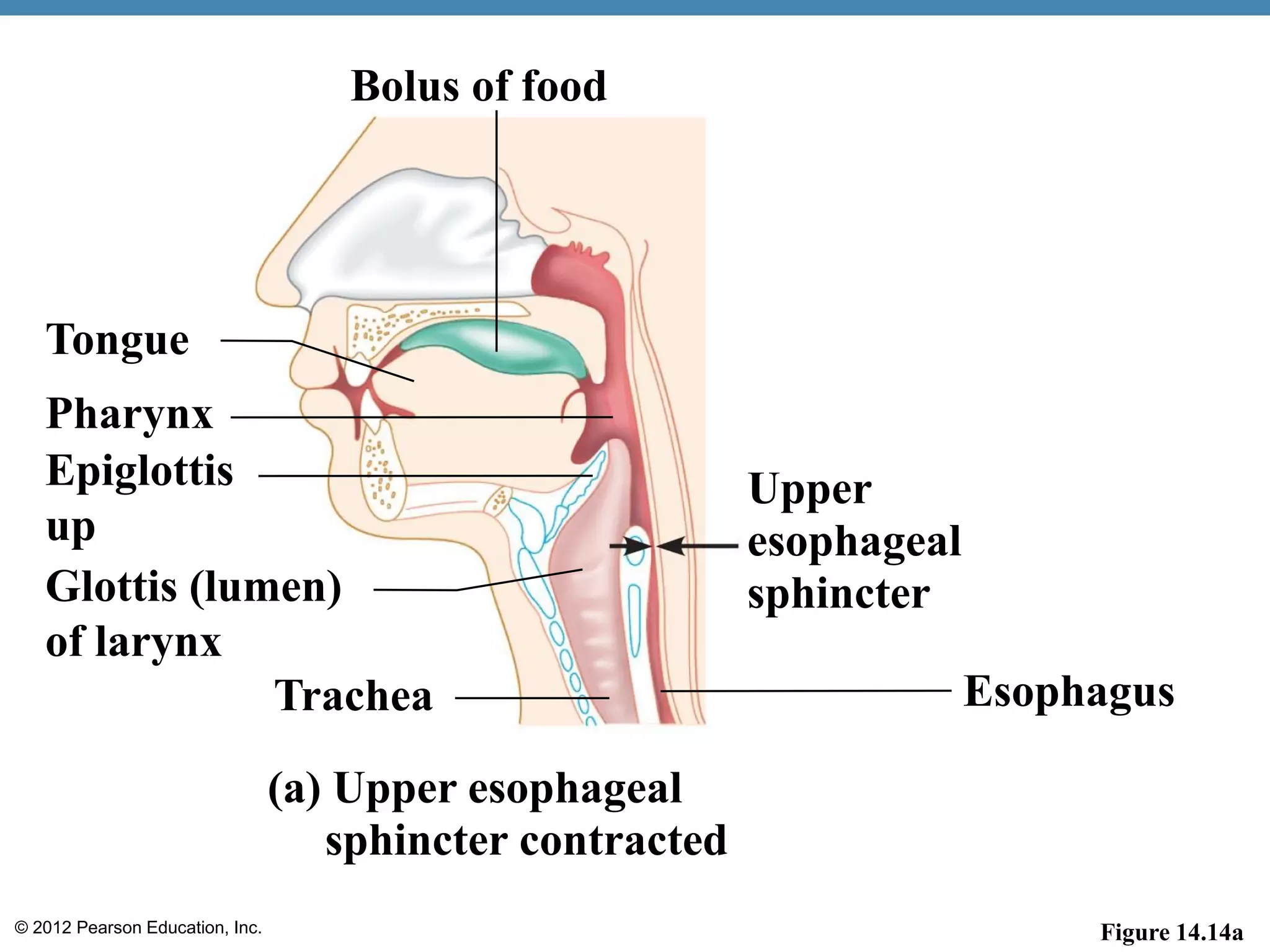
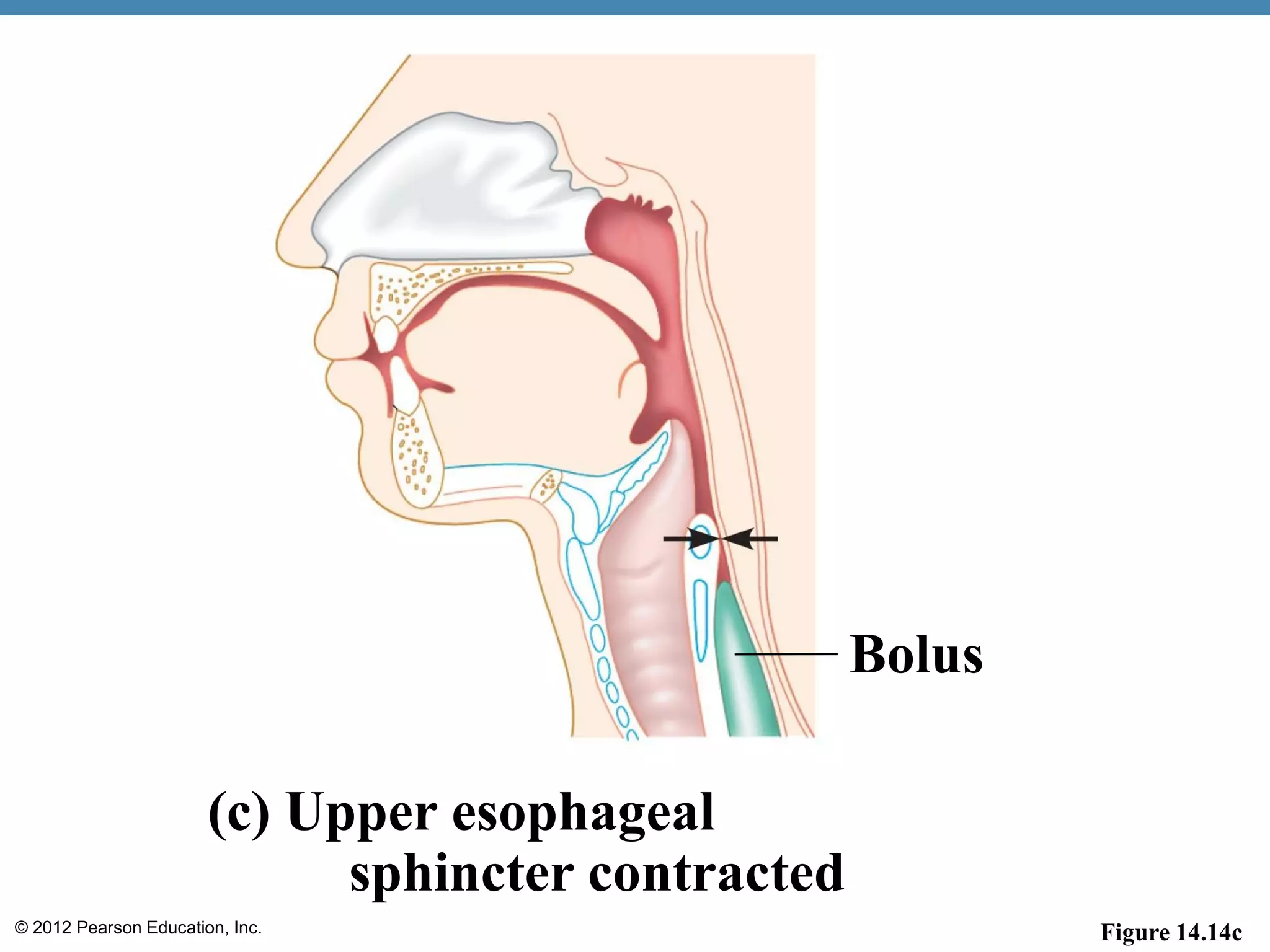
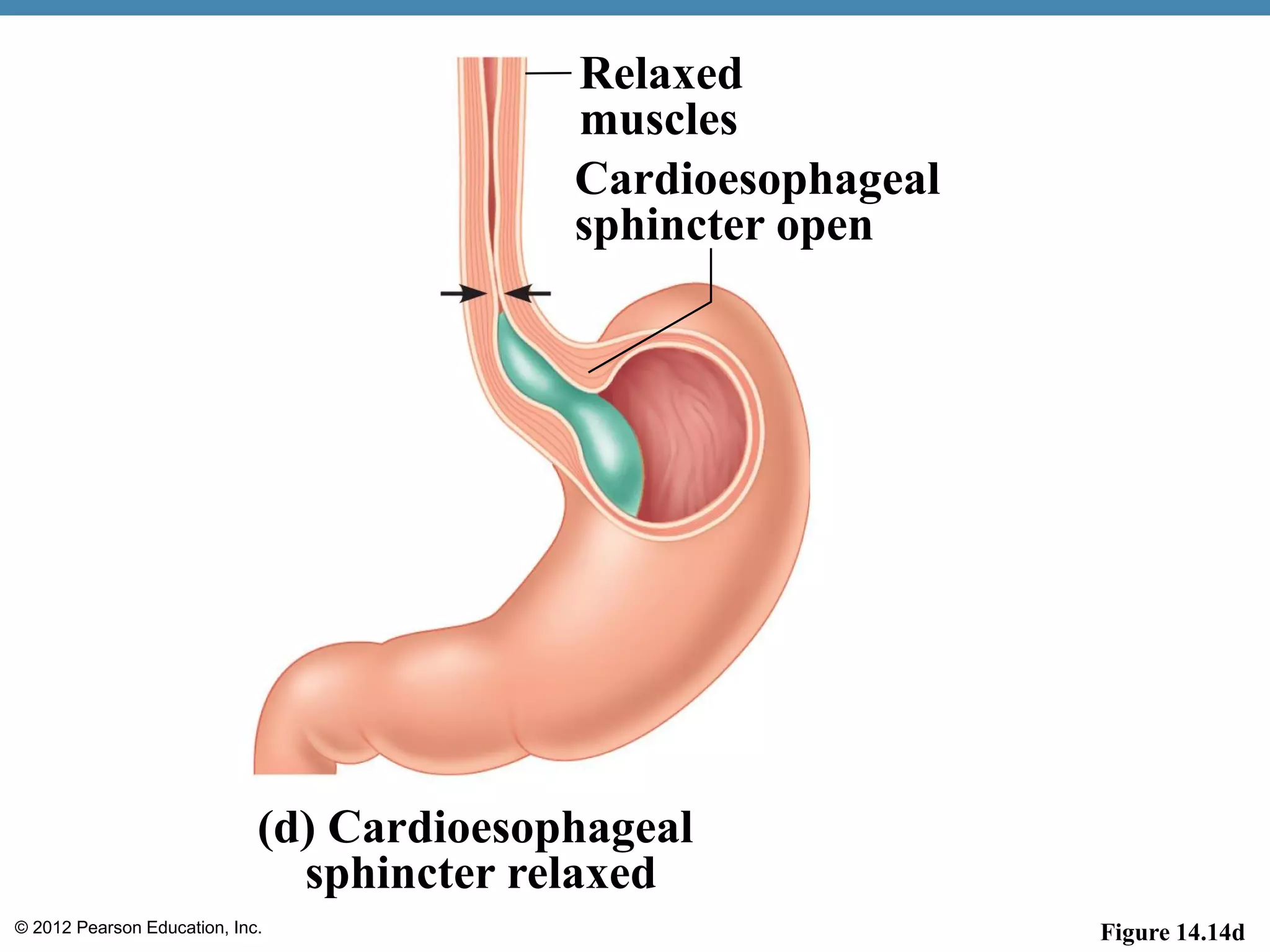
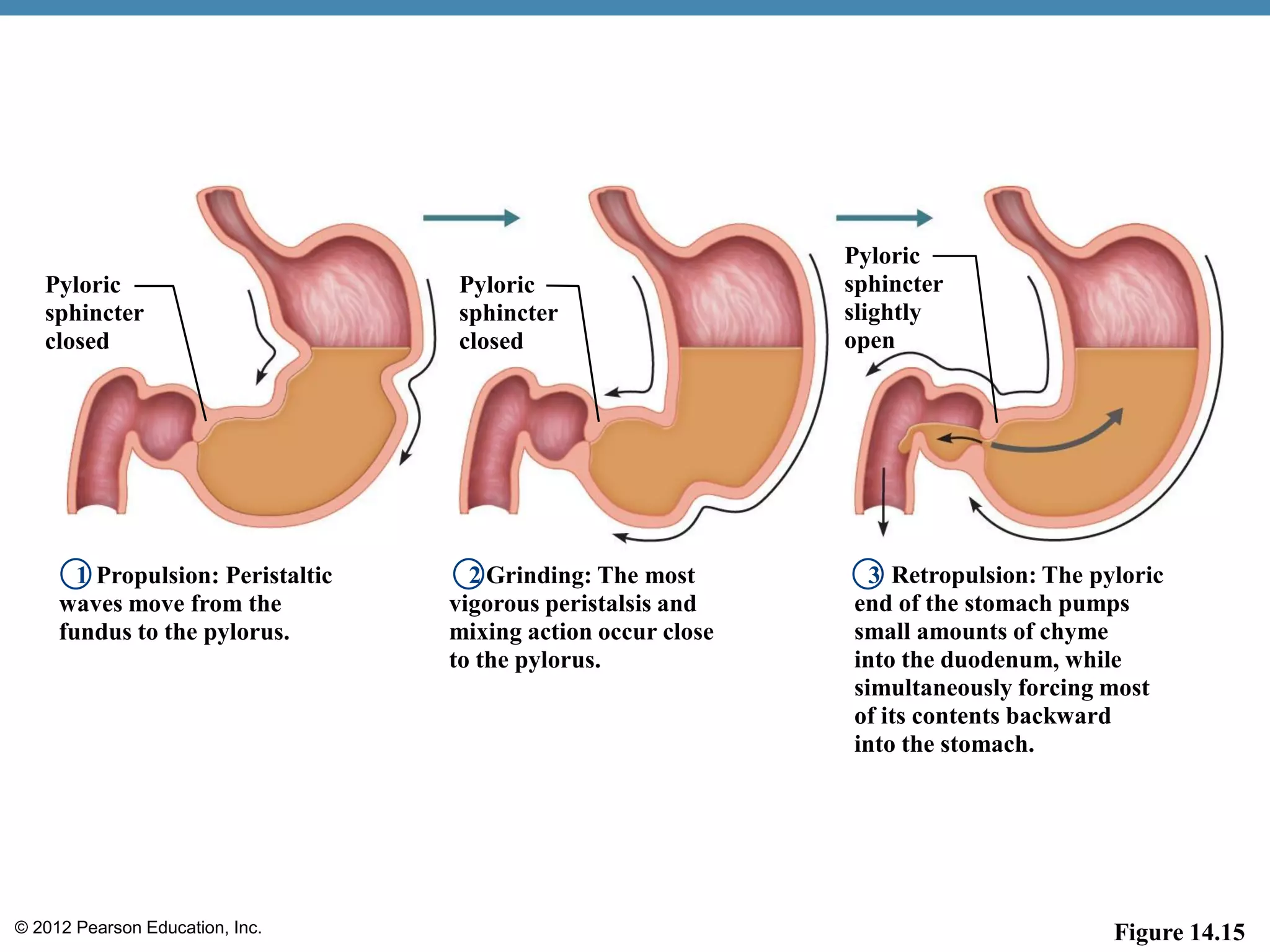
This document provides an overview of the structure and function of the human digestive system. It describes the organs that make up the digestive tract, including the mouth, esophagus, stomach, small intestine, large intestine and associated organs like the liver, gallbladder and pancreas. It explains the roles of these organs in ingestion, digestion, absorption and elimination and how they work together to break down food and extract nutrients for the body.