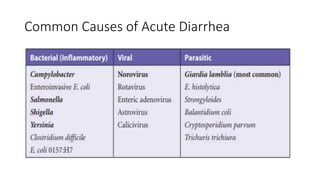
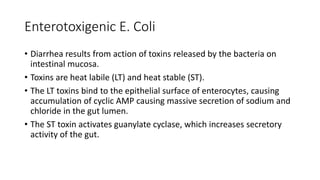
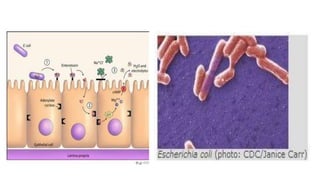
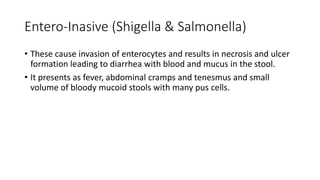
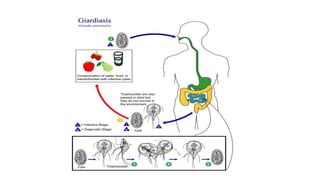
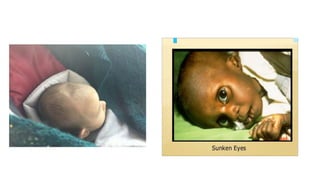
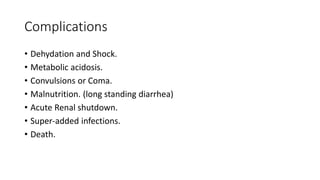
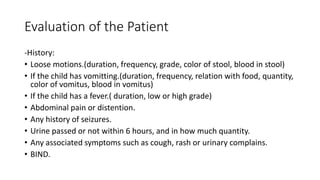
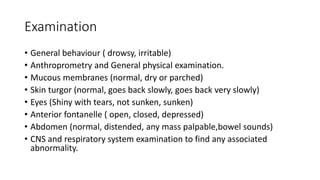
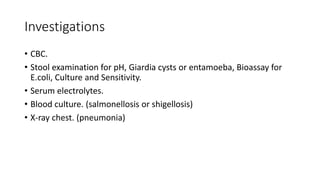
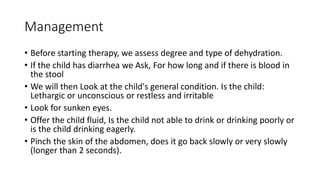
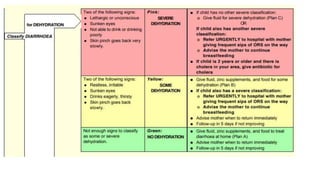
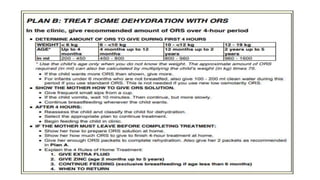
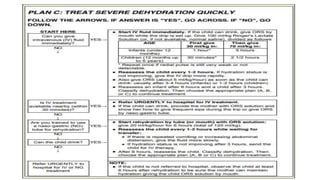
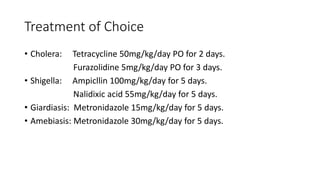
This document discusses acute diarrhea in children. It defines diarrhea and lists its leading causes as enterotoxigenic E. coli, enteroinvasive bacteria like Shigella and Salmonella, rotavirus, Vibrio cholerae, and Giardia lamblia. It describes the mechanisms by which these pathogens cause diarrhea and outlines their clinical presentations. The document also covers factors that increase susceptibility to diarrhea, effects of dehydration, evaluation of patients, management of rehydration, and treatment for specific causes.