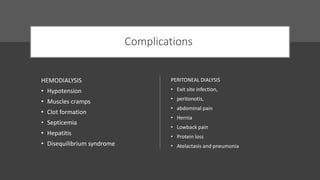
Hemodialysis involves removing waste and excess fluid from the blood of patients with kidney failure. It is done 3 times a week, with each session lasting 2-4 hours. Blood passes through a dialyzer containing semipermeable membranes where waste diffuses out of the blood into the dialysate solution. Ultrafiltration also removes fluid. Vascular access via fistula or graft is required. Nursing responsibilities include monitoring for hypotension and ensuring proper access care and dietary education. Peritoneal dialysis uses the peritoneal membrane and involves exchanging dialysate fluid in the abdomen via catheter.