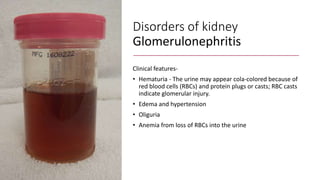
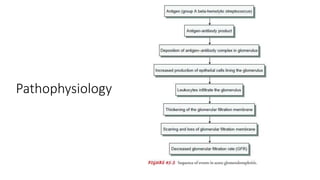
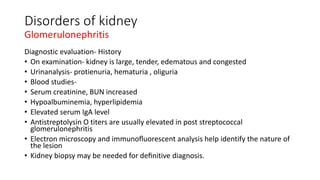
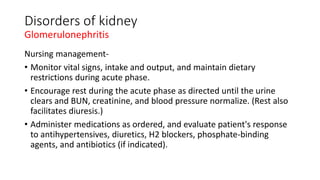
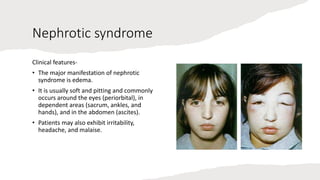
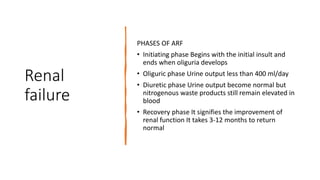
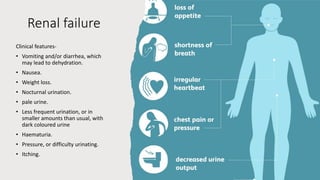
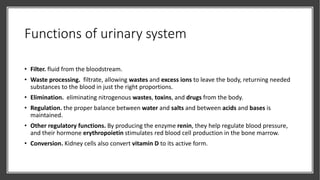
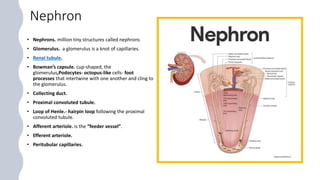
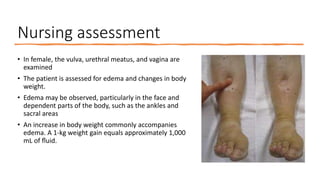
The document provides an overview of the nursing management of patients with genito-urinary system disorders, detailing urinary system functions, anatomy, and disorders such as glomerulonephritis and nephrotic syndrome. It discusses assessment techniques, clinical features, diagnostic evaluations, management strategies, and complications associated with these disorders. The focus is on promoting renal function and managing symptoms through both pharmacological and non-pharmacological approaches.

















![Disorders of kidney
Glomerulonephritis
Risk factors
• Group A beta- hemolytic streptococcal infection of
the throat
• Impetigo (infection of the skin)
• Acute viral infections- upper respiratory tract
infections, mumps, varicella zoster virus, Epstein-
Barr virus, hepatitis B, and human
immunodeficiency virus [HIV] infection).
• Antigens outside the body (eg, medications, foreign
serum)
• In other patients, the kidney tissue itself serves as
the inciting antigen.](https://image.slidesharecdn.com/genito-urinarysystemdisorders-1-220324080651/85/Genito-urinary-system-disorders-1-pptx-21-320.jpg)