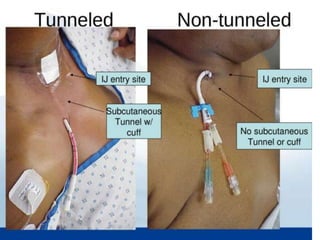
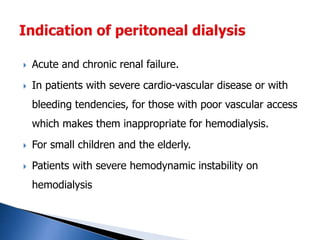
The document provides an overview of dialysis, primarily focusing on hemodialysis, its techniques, and applications for patients with end-stage renal disease (ESRD). It discusses various dialysis methods, vascular access options, and the importance of proper nursing responsibilities during dialysis procedures. Additionally, it highlights the role of levocarnitine in managing symptoms for hemodialysis patients and the differences between hemodialysis and peritoneal dialysis.