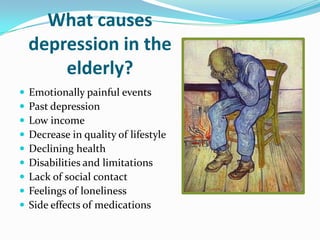
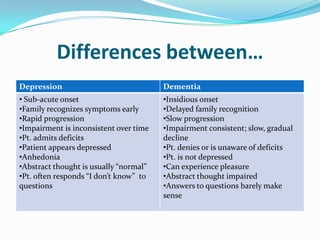
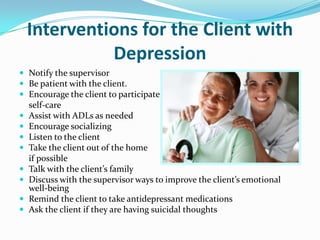
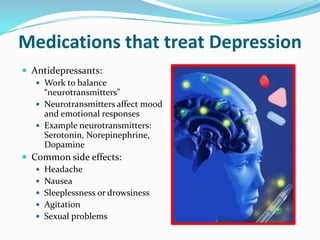
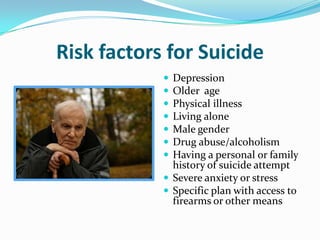
This document discusses depression in the elderly. It notes that over 2 million Americans over 65 suffer from depression, which is a mental illness and not a normal part of aging. Symptoms of depression include sadness, loss of interest in activities, changes in appetite and sleep, and thoughts of suicide. Depression in the elderly is often unrecognized and increases health risks. Causes can include painful life events, health issues, loneliness, and medication side effects. Caregivers are told to monitor clients for depression and suicidal thoughts, encourage socialization and activities, and ensure clients receive treatment which may include antidepressant medication.