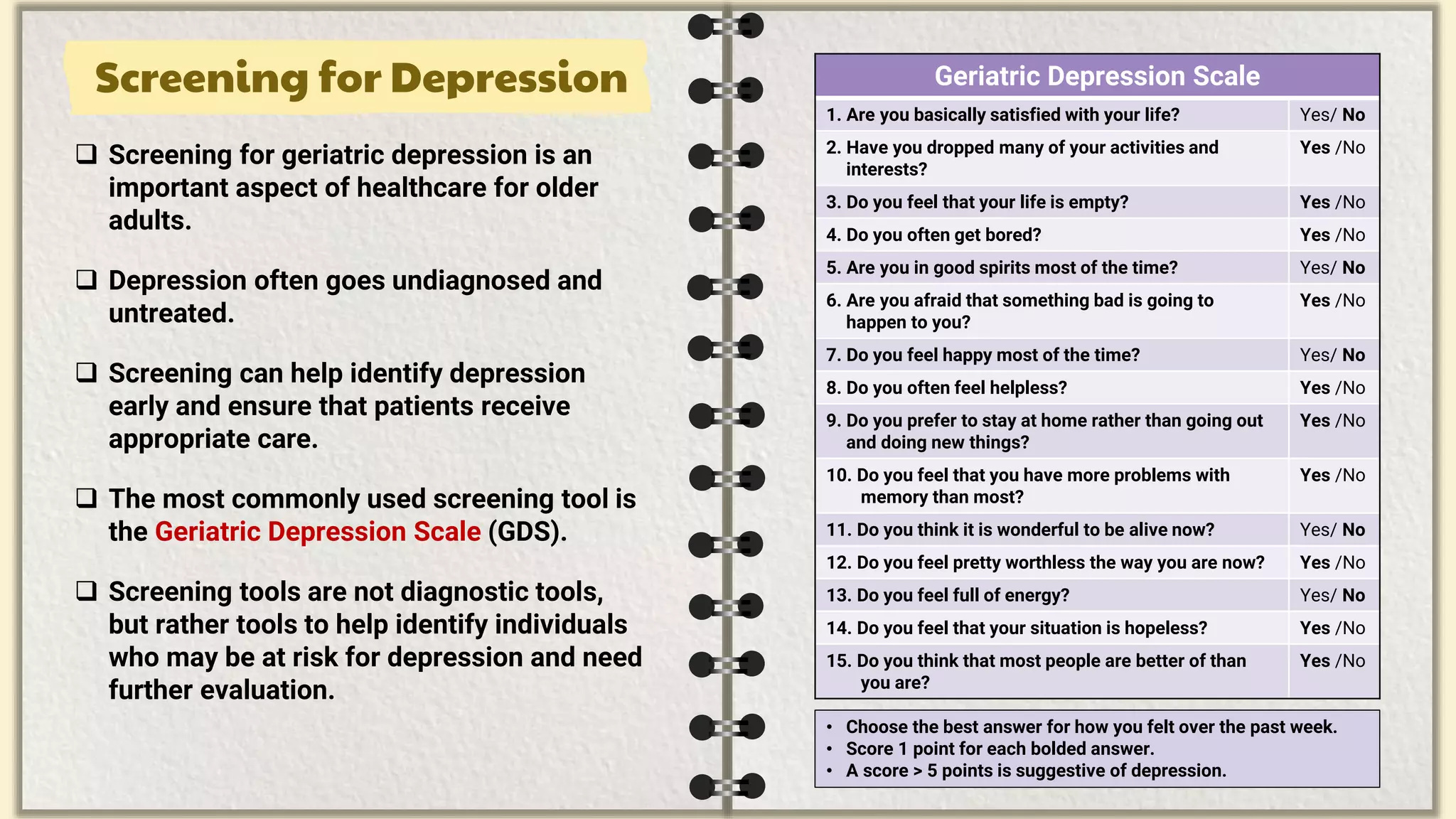
The document is a comprehensive guide on the prevalence, risk factors, clinical features, diagnosis, and management of depression in elderly patients. It highlights the importance of understanding the unique presentation of depression in this population and emphasizes the need for proper screening and tailored treatment strategies, considering pharmacological and non-pharmacological approaches. The guide also discusses common challenges in diagnosing depression in older adults and provides recommendations for effective management and treatment options.