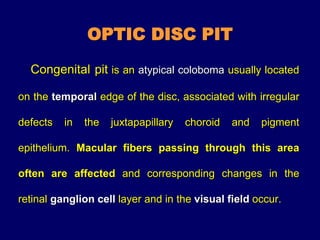
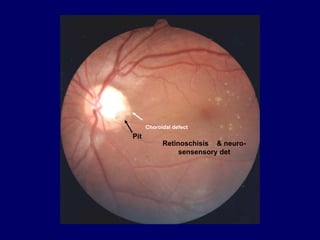
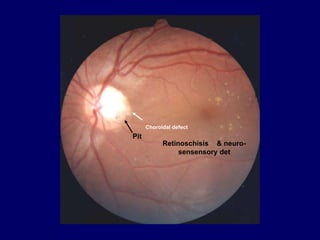
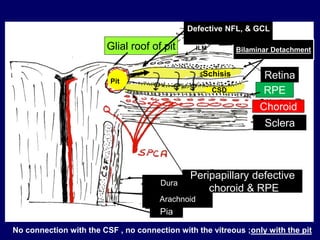
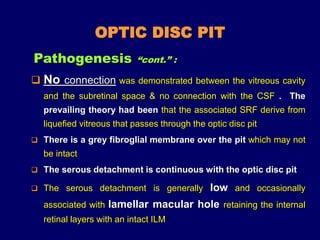
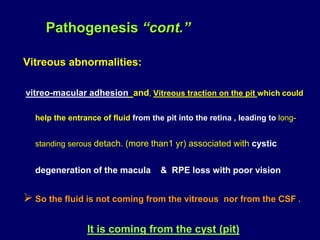
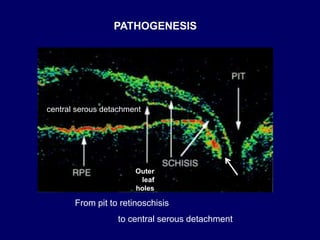
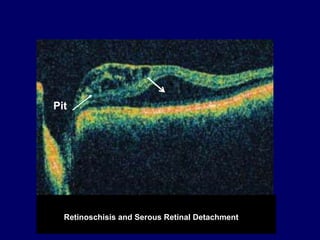
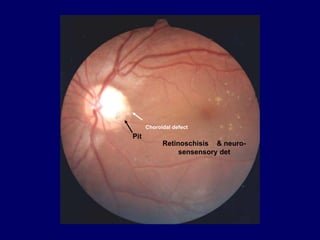
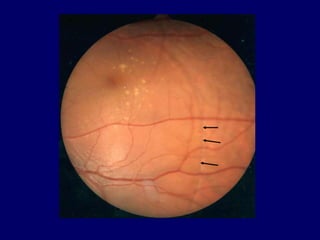
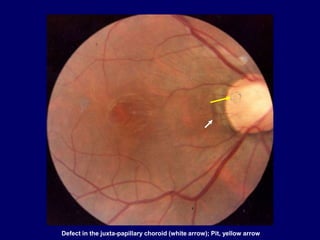
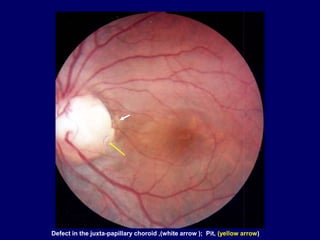
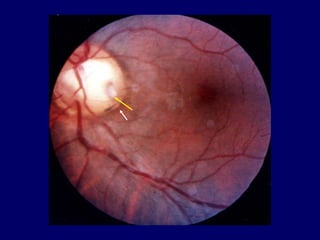
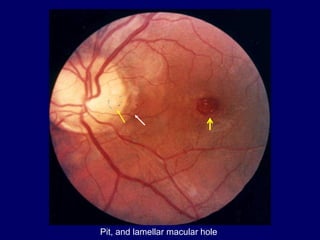
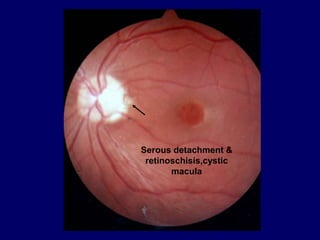
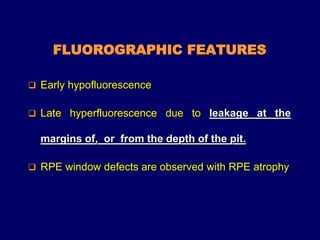
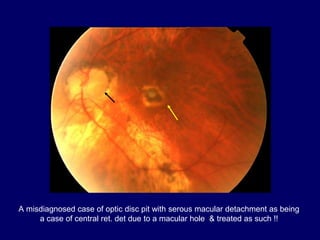
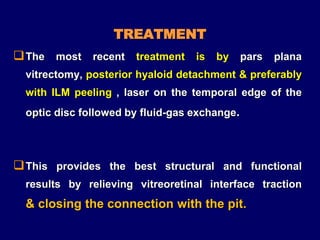
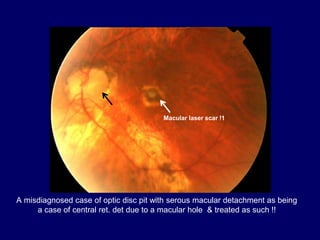
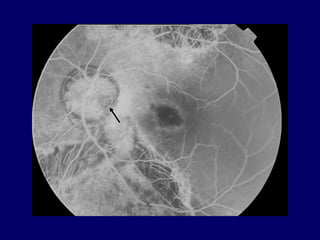
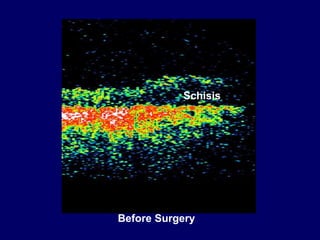
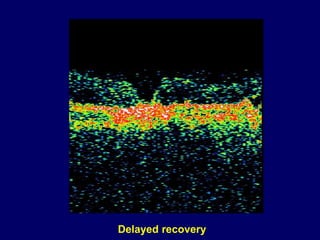
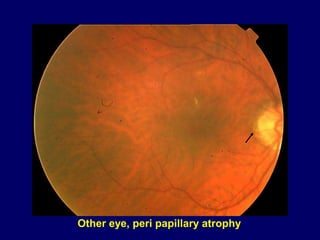
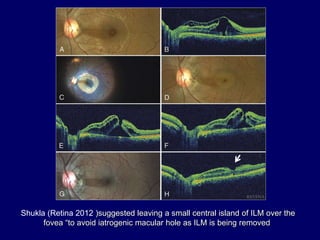
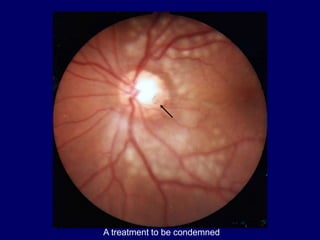
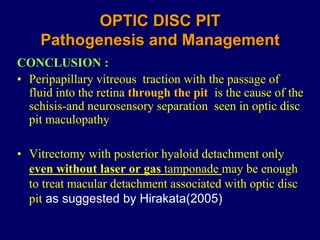
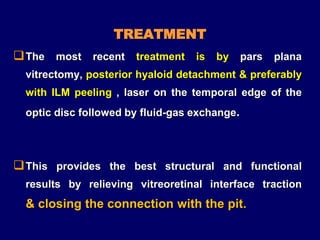
The document discusses optic disc pit, a rare congenital condition characterized by a defect usually located on the temporal edge of the optic disc, which can lead to various retinal issues, including retinoschisis and sensory macular detachments. Recent studies highlight the pathogenesis involving vitreous traction and fluid movement from the pit into the retina, and treatment options include vitrectomy and laser interventions to address retinal detachments. The conclusion emphasizes that relieving vitreoretinal interface traction can effectively manage the associated retinal complications.